Search
- Page Path
- HOME > Search
- Thyroid
- Prognostic Roles of Inflammatory Biomarkers in Radioiodine-Refractory Thyroid Cancer Treated with Lenvatinib
- Chae A Kim, Mijin Kim, Meihua Jin, Hee Kyung Kim, Min Ji Jeon, Dong Jun Lim, Bo Hyun Kim, Ho-Cheol Kang, Won Bae Kim, Dong Yeob Shin, Won Gu Kim
- Endocrinol Metab. 2024;39(2):334-343. Published online April 4, 2024
- DOI: https://doi.org/10.3803/EnM.2023.1854

- 333 View
- 24 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Inflammatory biomarkers, such as the neutrophil-to-lymphocyte ratio (NLR), lymphocyte-to-monocyte ratio (LMR), and platelet-to-lymphocyte ratio (PLR), serve as valuable prognostic indicators in various cancers. This multicenter, retrospective cohort study assessed the treatment outcomes of lenvatinib in 71 patients with radioactive iodine (RAI)-refractory thyroid cancer, considering the baseline inflammatory biomarkers.
Methods
This study retrospectively included patients from five tertiary hospitals in Korea whose complete blood counts were available before lenvatinib treatment. Progression-free survival (PFS) and overall survival (OS) were evaluated based on the median value of inflammatory biomarkers.
Results
No significant differences in baseline characteristics were observed among patients grouped according to the inflammatory biomarkers, except for older patients with a higher-than-median NLR (≥2) compared to their counterparts with a lower NLR (P= 0.01). Patients with a higher-than-median NLR had significantly shorter PFS (P=0.02) and OS (P=0.017) than those with a lower NLR. In multivariate analysis, a higher-than-median NLR was significantly associated with poor OS (hazard ratio, 3.0; 95% confidence interval, 1.24 to 7.29; P=0.015). However, neither the LMR nor the PLR was associated with PFS. A higher-than-median LMR (≥3.9) was significantly associated with prolonged OS compared to a lower LMR (P=0.036). In contrast, a higher-than-median PLR (≥142.1) was associated with shorter OS compared to a lower PLR (P=0.039).
Conclusion
Baseline inflammatory biomarkers can serve as predictive indicators of PFS and OS in patients with RAI-refractory thyroid cancer treated with lenvatinib.

- Thyroid
- Active Surveillance for Low-Risk Papillary Thyroid Carcinoma as an Acceptable Management Option with Additional Benefits: A Comprehensive Systematic Review
- Jee Hee Yoon, Wonsuk Choi, Ji Yong Park, A Ram Hong, Hee Kyung Kim, Ho-Cheol Kang
- Endocrinol Metab. 2024;39(1):152-163. Published online January 22, 2024
- DOI: https://doi.org/10.3803/EnM.2023.1794
- 1,152 View
- 42 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
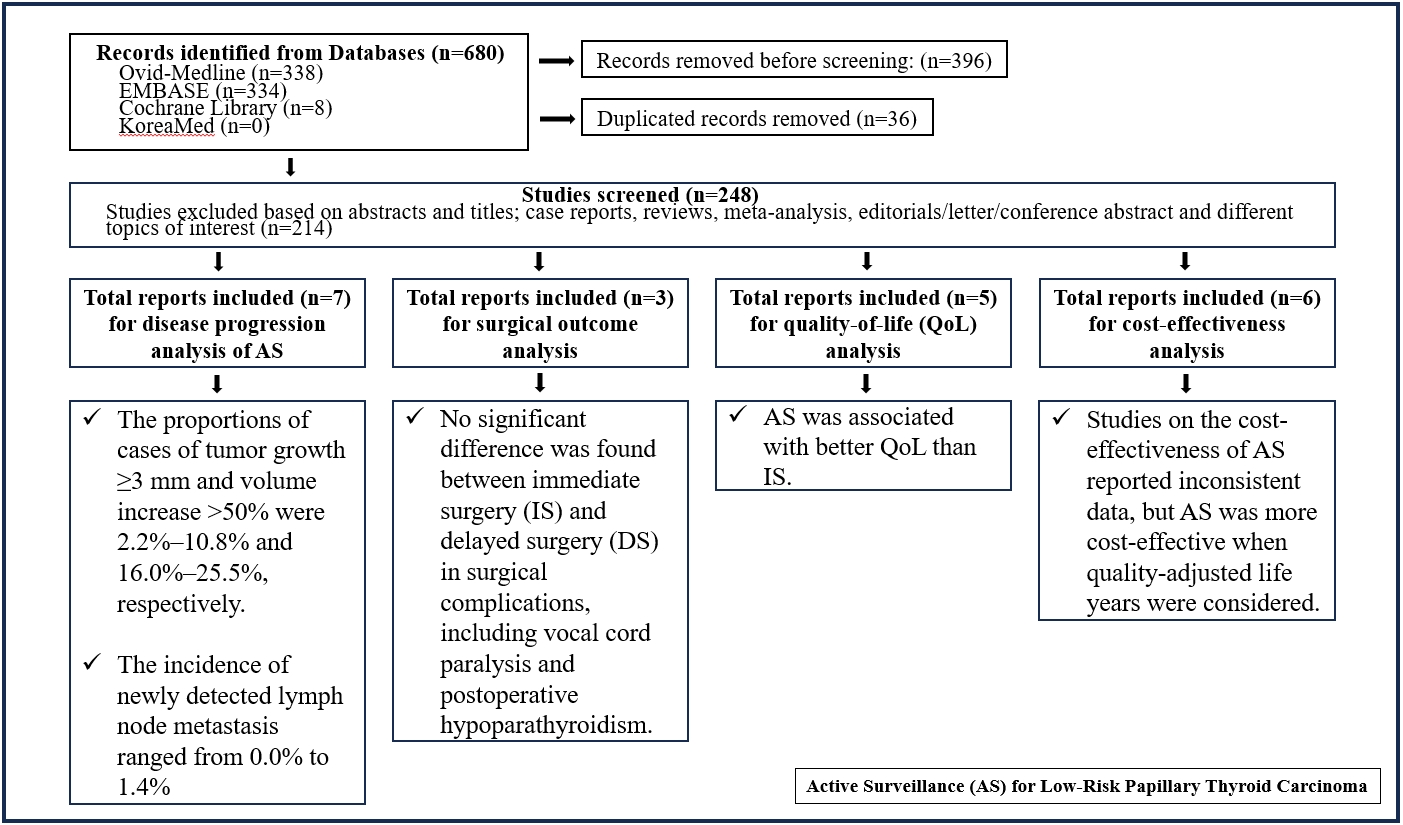
Active surveillance (AS) has been introduced as a management strategy for low-risk papillary thyroid carcinoma (PTC) due to its typically indolent nature. Despite this, the widespread adoption of AS has encountered several challenges. The aim of this systematic review was to evaluate the safety of AS related to disease progression and its benefits compared with immediate surgery (IS).
Methods
Studies related to AS in patients with low-risk PTC were searched through the Ovid MEDLINE, Embase, Cochrane Library, and KoreaMed databases. Studies on disease progression, surgical complication, quality of life (QoL), and cost-effectiveness were separately analyzed and narratively synthesized.
Results
In the evaluation of disease progression, the proportions of cases with tumor growth ≥3 mm and a volume increase >50% were 2.2%–10.8% and 16.0%–25.5%, respectively. Newly detected lymph node metastasis was identified in 0.0%–1.4% of patients. No significant difference was found between IS and delayed surgery in surgical complications, including vocal cord paralysis and postoperative hypoparathyroidism. AS was associated with better QoL than IS. Studies on the cost-effectiveness of AS reported inconsistent data, but AS was more cost-effective when quality-adjusted life years were considered.
Conclusion
AS is an acceptable management option for patients with low-risk PTC based on the low rate of disease progression and the absence of an increased mortality risk. AS has additional benefits, including improved QoL and greater QoL-based cost-effectiveness. -
Citations
Citations to this article as recorded by- It Is Time to Understand the Additional Benefits of Active Surveillance for Low-Risk Papillary Thyroid Carcinoma
Kyeong Jin Kim
Endocrinology and Metabolism.2024; 39(1): 95. CrossRef
- It Is Time to Understand the Additional Benefits of Active Surveillance for Low-Risk Papillary Thyroid Carcinoma

- Thyroid
Thyroid Cancer Screening - A Comprehensive Assessment of the Harms of Fine-Needle Aspiration Biopsy for Thyroid Nodules: A Systematic Review
- Ji Yong Park, Wonsuk Choi, A Ram Hong, Jee Hee Yoon, Hee Kyung Kim, Ho-Cheol Kang
- Endocrinol Metab. 2023;38(1):104-116. Published online February 27, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1669
- 3,648 View
- 161 Download
- 4 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
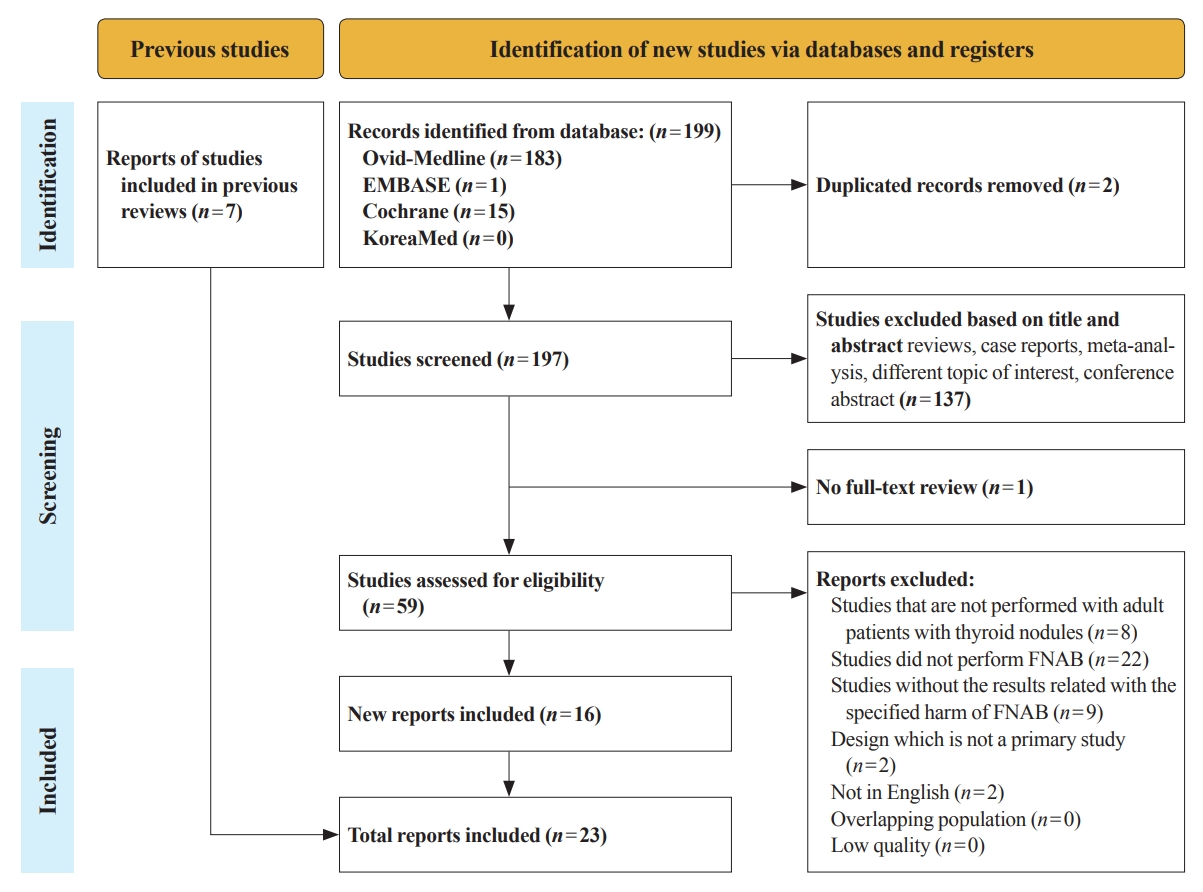
There have concerns related with the potential harms of fine-needle aspiration biopsy (FNAB). We aimed to summarize the clinical complications and evaluate the safety of FNAB.
Methods
Studies related with the harms of FNAB were searched on MEDLINE, Embase, Cochrane library, and KoreaMed from 2012 to 2022. Also, studies reviewed in the previous systematic reviews were evaluated. Included clinical complications were postprocedural pain, bleeding events, neurological symptoms, tracheal puncture, infections, post-FNAB thyrotoxicosis, and needle tract implantation of thyroid cancers.
Results
Twenty-three cohort studies were included in this review. Nine studies which were related with FNAB-related pain showed that most of the subjects had no or mild discomfort. The 0% to 6.4% of the patients had hematoma or hemorrhage after FNAB, according to 15 studies. Vasovagal reaction, vocal cord palsy, and tracheal puncture have rarely described in the included studies. Needle tract implantation of thyroid malignancies was described in three studies reporting 0.02% to 0.19% of the incidence rate.
Conclusion
FNAB is considered to be a safe diagnostic procedure with rare complications, which are mainly minor events. Thorough assessement of the patients’ medical condition when deciding to perform FNABs would be advisable to lower potential complications. -
Citations
Citations to this article as recorded by- A Narrative Review of the 2023 Korean Thyroid Association Management Guideline for Patients with Thyroid Nodules
Eun Kyung Lee, Young Joo Park, Chan Kwon Jung, Dong Gyu Na
Endocrinology and Metabolism.2024; 39(1): 61. CrossRef - Fine-needle aspiration cytology for neck lesions in patients with antithrombotic/anticoagulant medications: systematic review and meta-analysis
Dongbin Ahn, Ji Hye Kwak, Gill Joon Lee, Jin Ho Sohn
European Radiology.2024;[Epub] CrossRef - To Screen or Not to Screen?
Do Joon Park
Endocrinology and Metabolism.2023; 38(1): 69. CrossRef - Thyroid Cancer Screening: How to Maximize Its Benefits and Minimize Its Harms
Jung Hwan Baek
Endocrinology and Metabolism.2023; 38(1): 75. CrossRef - Evaluation of the Appropriateness of Thyroid Fine-Needle Aspiration
Lairce Cristina Ribeiro Brito, Iara Beatriz De Carvalho Botêlho, Lanna Matos Silva Fernandes, Nayze Lucena Sangreman Aldeman, Uziel Nunes Silva
International Journal for Innovation Education and Research.2023; 11(6): 8. CrossRef
- A Narrative Review of the 2023 Korean Thyroid Association Management Guideline for Patients with Thyroid Nodules

- Miscellaneous
- Immune Checkpoint Inhibitors and Endocrine Disorders: A Position Statement from the Korean Endocrine Society
- Hyemi Kwon, Eun Roh, Chang Ho Ahn, Hee Kyung Kim, Cheol Ryong Ku, Kyong Yeun Jung, Ju Hee Lee, Eun Heui Kim, Sunghwan Suh, Sangmo Hong, Jeonghoon Ha, Jun Sung Moon, Jin Hwa Kim, Mi-kyung Kim, The Committee of Clinical Practice Guideline of the Korean Endocrine Society
- Endocrinol Metab. 2022;37(6):839-850. Published online December 26, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1627
- 3,488 View
- 321 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
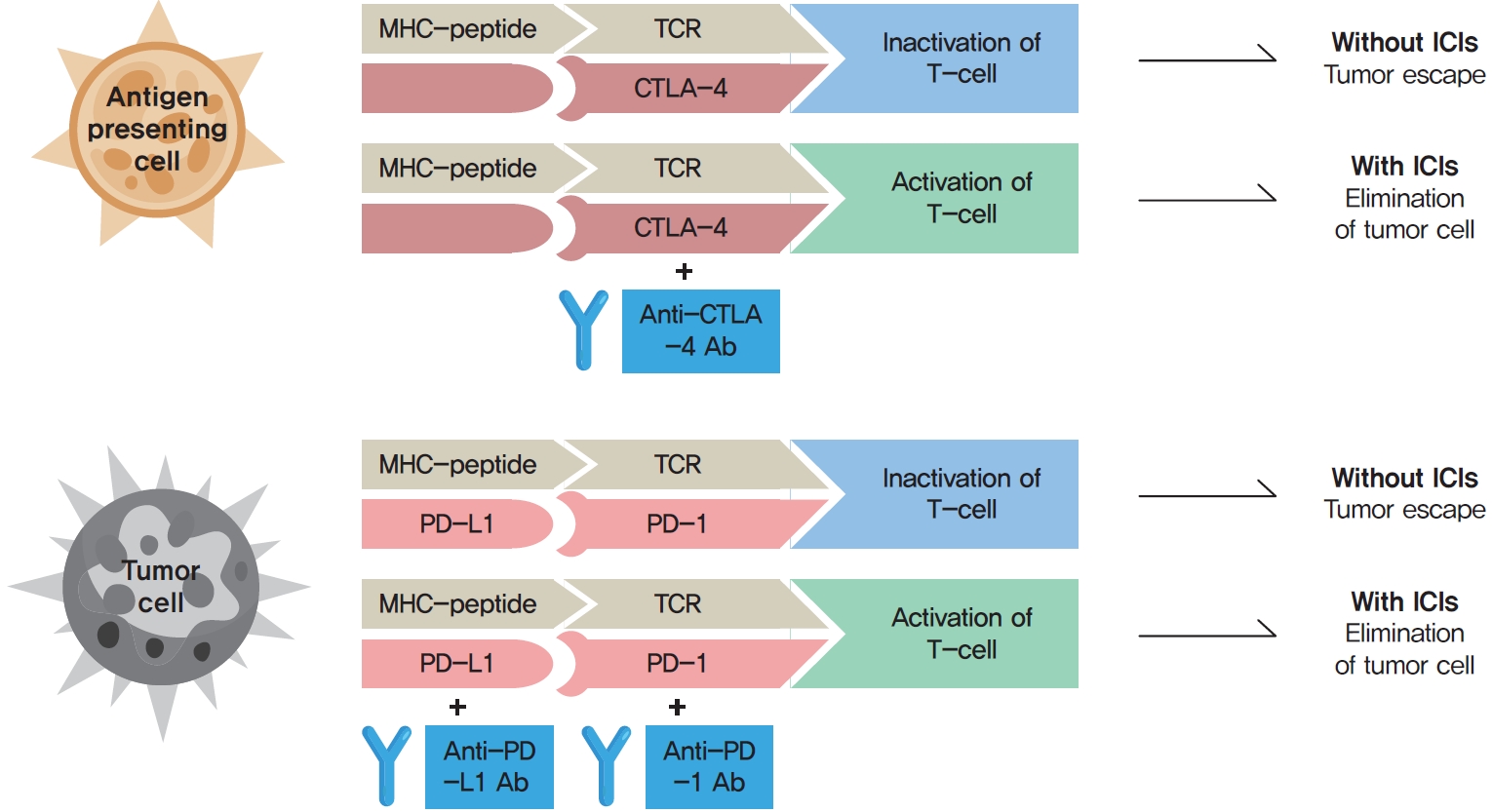
ePub - Immune checkpoint inhibitors (ICIs) including an anti-cytotoxic T-lymphocyte-associated antigen 4 inhibitor, anti-programmed cell death protein 1 (PD-1) inhibitors, and anti-PD-ligand 1 inhibitors are representative therapeutics for various malignancies. In oncology, the application of ICIs is currently expanding to a wider range of malignancies due to their remarkable clinical outcomes. ICIs target immune checkpoints which suppress the activity of T-cells that are specific for tumor antigens, thereby allowing tumor cells to escape the immune response. However, immune checkpoints also play a crucial role in preventing autoimmune reactions. Therefore, ICIs targeting immune checkpoints can trigger various immune-related adverse events (irAEs), especially in endocrine organs. Considering the endocrine organs that are frequently involved, irAEs associated endocrinopathies are frequently life-threatening and have unfavorable clinical implications for patients. However, there are very limited data from large clinical trials that would inform the development of clinical guidelines for patients with irAEs associated endocrinopathies. Considering the current clinical situation, in which the scope and scale of the application of ICIs are increasing, position statements from clinical specialists play an essential role in providing the appropriate recommendations based on both medical evidence and clinical experience. As endocrinologists, we would like to present precautions and recommendations for the management of immune-related endocrine disorders, especially those involving the adrenal, thyroid, and pituitary glands caused by ICIs.
-
Citations
Citations to this article as recorded by- Pembrolizumab plus lenvatinib for radically unresectable or metastatic renal cell carcinoma in the Japanese population
Ryo Fujiwara, Takeshi yuasa, kenichi kobayashi, tetsuya yoshida, susumu kageyama
Expert Review of Anticancer Therapy.2023; 23(5): 461. CrossRef - Incidence of Endocrine-Related Dysfunction in Patients Treated with New Immune Checkpoint Inhibitors: A Meta-Analysis and Comprehensive Review
Won Sang Yoo, Eu Jeong Ku, Eun Kyung Lee, Hwa Young Ahn
Endocrinology and Metabolism.2023; 38(6): 750. CrossRef
- Pembrolizumab plus lenvatinib for radically unresectable or metastatic renal cell carcinoma in the Japanese population

- Thyroid
- Clinical Characteristics and Prognosis of Coexisting Thyroid Cancer in Patients with Graves’ Disease: A Retrospective Multicenter Study
- Jee Hee Yoon, Meihua Jin, Mijin Kim, A Ram Hong, Hee Kyung Kim, Bo Hyun Kim, Won Bae Kim, Young Kee Shong, Min Ji Jeon, Ho-Cheol Kang
- Endocrinol Metab. 2021;36(6):1268-1276. Published online November 26, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1227
- 4,837 View
- 186 Download
- 10 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
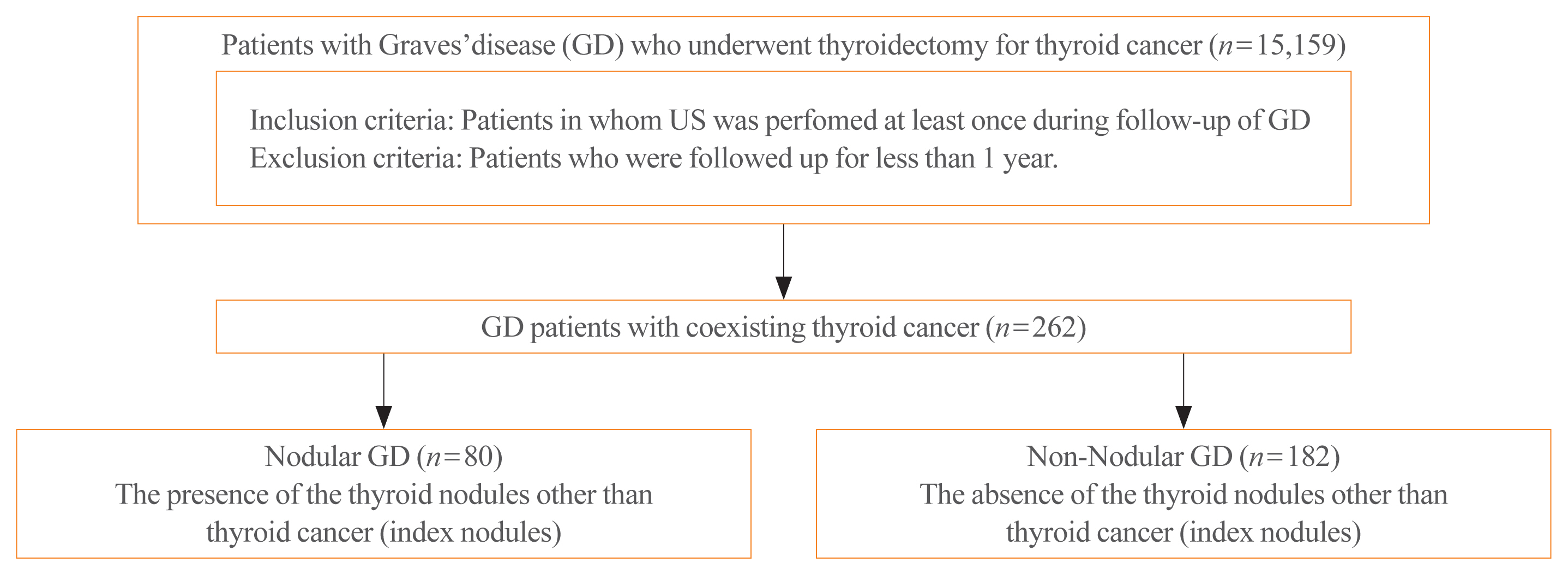
The association between Graves’ disease (GD) and co-existing thyroid cancer is still controversial and most of the previously reported data have been based on surgically treated GD patients. This study investigated the clinicopathological findings and prognosis of concomitant thyroid cancer in GD patients in the era of widespread application of ultrasonography.
Methods
Data of GD patients who underwent thyroidectomy for thyroid cancer between 2010 and 2019 in three tertiary hospitals in South Korea (Asan Medical Center, Chonnam National University Hwasun Hospital, and Pusan National University Hospital) were collected and analyzed retrospectively. In the subgroup analysis, aggressiveness and clinical outcomes of thyroid cancer were compared nodular GD and non-nodular GD groups according to the presence or absence of the thyroid nodules other than thyroid cancer (index nodules).
Results
Of the 15,159 GD patients treated at the hospitals during the study period, 262 (1.7%) underwent thyroidectomy for coexisting thyroid cancer. Eleven patients (4.2%) were diagnosed with occult thyroid cancer and 182 patients (69.5%) had microcarcinomas. No differences in thyroid cancer aggressiveness, ultrasonographic findings, or prognosis were observed between the nodular GD and non-nodular GD groups except the cancer subtype. In the multivariate analysis, only lymph node (LN) metastasis was an independent prognostic factor for recurrent/persistent disease of thyroid cancer arising in GD (P=0.020).
Conclusion
The prevalence of concomitant thyroid cancer in GD patients was considerably lower than in previous reports. The clinical outcomes of thyroid cancer in GD patients were also excellent but, more cautious follow-up is necessary for patients with LN metastasis in the same way as for thyroid cancer in non-GD patients. -
Citations
Citations to this article as recorded by- Comparison of Surgical Outcomes of Transoral Versus Open Thyroidectomy for Graves Disease
Suo-Hsien Wang, Wu-Po Chao, Ta-You Lo, Soh-Ching Ng, Yu-Hsien Chen
Surgical Laparoscopy, Endoscopy & Percutaneous Techniques.2024; 34(2): 150. CrossRef - Outcomes of Surgical Treatment for Graves’ Disease: A Single-Center Experience of 216 Cases
Hanxing Sun, Hui Tong, Xiaohui Shen, Haoji Gao, Jie Kuang, Xi Chen, Qinyu Li, Weihua Qiu, Zhuoran Liu, Jiqi Yan
Journal of Clinical Medicine.2023; 12(4): 1308. CrossRef - Cancer and Mortality Risks of Graves’ Disease in South Korea Based on National Data from 2010 to 2019
Young Ju Choi, Kyungdo Han, Won Kyoung Cho, Min Ho Jung, Byung-Kyu Suh
Clinical Epidemiology.2023; Volume 15: 535. CrossRef - Risk and Prognosis of Thyroid Cancer in Patients with Graves’ Disease: An Umbrella Review
Marco Palella, Francesca Maria Giustolisi, Adriana Modica Fiascaro, Martina Fichera, Antonella Palmieri, Rossella Cannarella, Aldo E. Calogero, Margherita Ferrante, Maria Fiore
Cancers.2023; 15(10): 2724. CrossRef - Characteristics, staging and outcomes of differentiated thyroid cancer in patients with and without Graves’ disease
Chaitra Gopinath, Hanna Crow, Sujata Panthi, Leonidas Bantis, Kenneth D. Burman, Chitra Choudhary
Journal of Clinical & Translational Endocrinology.2023; 33: 100321. CrossRef - Prevalence, Treatment Status, and Comorbidities of Hyperthyroidism in Korea from 2003 to 2018: A Nationwide Population Study
Hwa Young Ahn, Sun Wook Cho, Mi Young Lee, Young Joo Park, Bon Seok Koo, Hang-Seok Chang, Ka Hee Yi
Endocrinology and Metabolism.2023; 38(4): 436. CrossRef - Hashimoto’s Thyroiditis and Papillary Thyroid Carcinoma: A Follow-Up Study in Patients with Absence of Aggressive Risk Factors at the Surgery of the Primary Tumor
Andrea Marongiu, Susanna Nuvoli, Andrea De Vito, Sonia Vargiu, Angela Spanu, Giuseppe Madeddu
Diagnostics.2023; 13(19): 3068. CrossRef - Table of Contents
Clinical Thyroidology.2022; 34(2): 48. CrossRef - Predisposition to and Prognosis of Thyroid Cancer May Not Be Affected by Graves’ Disease, But Some Questions Still Remain
Yanrui Huang, Haixia Guan
Clinical Thyroidology.2022; 34(2): 59. CrossRef - A Comparative Follow-Up Study of Patients with Papillary Thyroid Carcinoma Associated or Not with Graves’ Disease
Andrea Marongiu, Susanna Nuvoli, Andrea De Vito, Maria Rondini, Angela Spanu, Giuseppe Madeddu
Diagnostics.2022; 12(11): 2801. CrossRef - An unusual case of papillary thyroid carcinoma presenting as Graves’ disease
Pooja Tiwari, Uma Kaimal Saikia, Abhamoni Baro, Ashok Krishna Bhuyan
Thyroid Research and Practice.2022; 19(1): 47. CrossRef
- Comparison of Surgical Outcomes of Transoral Versus Open Thyroidectomy for Graves Disease

- Thyroid
- Clinicopathological Characteristics and Disease-Free Survival in Patients with Hürthle Cell Carcinoma: A Multicenter Cohort Study in South Korea
- Meihua Jin, Eun Sook Kim, Bo Hyun Kim, Hee Kyung Kim, Yea Eun Kang, Min Ji Jeon, Tae Yong Kim, Ho-Cheol Kang, Won Bae Kim, Young Kee Shong, Mijin Kim, Won Gu Kim
- Endocrinol Metab. 2021;36(5):1078-1085. Published online October 28, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1151
- 3,880 View
- 110 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Hürthle cell carcinoma (HCC), a type of thyroid carcinoma, is rare in South Korea, and few studies have investigated its prognosis.
Methods
This long-term multicenter retrospective cohort study evaluated the clinicopathological features and clinical outcomes in patients with HCC who underwent thyroid surgery between 1996 and 2009.
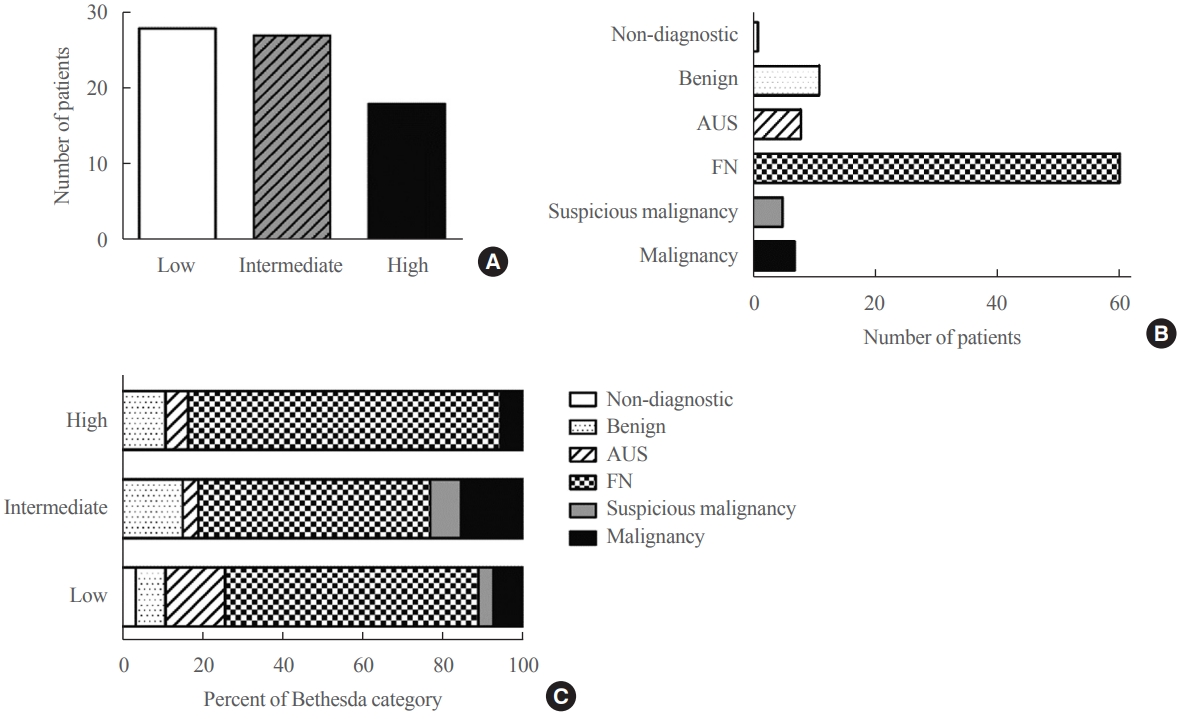
Results
The mean age of the 97 patients included in the study was 50.3 years, and 26.8% were male. The mean size of the primary tumor was 3.2±1.8 cm, and three (3.1%) patients had distant metastasis at initial diagnosis. Ultrasonographic findings were available for 73 patients; the number of nodules with low-, intermediate-, and high suspicion was 28 (38.4%), 27 (37.0%), and 18 (24.7%), respectively, based on the Korean-Thyroid Imaging Reporting and Data System. Preoperatively, follicular neoplasm (FN) or suspicion for FN accounted for 65.2% of the cases according to the Bethesda category, and 13% had malignancy or suspicious for malignancy. During a median follow-up of 8.5 years, eight (8.2%) patients had persistent/recurrent disease, and none died of HCC. Older age, gross extrathyroidal extension (ETE), and widely invasive types of tumors were significantly associated with distant metastasis (all P<0.01). Gross ETE (hazard ratio [HR], 27.7; 95% confidence interval [CI], 2.2 to 346.4; P=0.01) and widely invasive classification (HR, 6.5; 95% CI, 1.1 to 39.4; P=0.04) were independent risk factors for poor disease-free survival (DFS).
Conclusion
The long-term prognosis of HCC is relatively favorable in South Korea from this study, although this is not a nation-wide data, and gross ETE and widely invasive cancer are significant prognostic factors for DFS. The diagnosis of HCC by ultrasonography and cytopathology remains challenging. -
Citations
Citations to this article as recorded by- Molecular Alterations and Comprehensive Clinical Management of Oncocytic Thyroid Carcinoma
Lindsay A. Bischoff, Ian Ganly, Laura Fugazzola, Erin Buczek, William C. Faquin, Bryan R. Haugen, Bryan McIver, Caitlin P. McMullen, Kate Newbold, Daniel J. Rocke, Marika D. Russell, Mabel Ryder, Peter M. Sadow, Eric Sherman, Maisie Shindo, David C. Shonk
JAMA Otolaryngology–Head & Neck Surgery.2024; 150(3): 265. CrossRef - Oncocytic carcinoma of the thyroid: Conclusions from a 20‐year patient cohort
Nelson R. Gruszczynski, Shahzeb S. Hasan, Ana G. Brennan, Julian De La Chapa, Adithya S. Reddy, David N. Martin, Prem P. Batchala, Edward B. Stelow, Eric M. Dowling, Katherine L. Fedder, Jonathan C. Garneau, David C. Shonka
Head & Neck.2024;[Epub] CrossRef - Hurthle cell carcinoma: a rare variant of thyroid malignancy – a case report
Yuvraj Adhikari, Anupama Marasini, Nawaraj Adhikari, Laxman D. Paneru, Binit Upadhaya Regmi, Manita Raut
Annals of Medicine & Surgery.2023; 85(5): 1940. CrossRef - Hürthle Cell Carcinoma: Single Center Analysis and Considerations for Surgical Management Based on the Recent Literature
Costanza Chiapponi, Milan J.M. Hartmann, Matthias Schmidt, Michael Faust, Christiane J. Bruns, Anne M. Schultheis, Hakan Alakus
Frontiers in Endocrinology.2022;[Epub] CrossRef
- Molecular Alterations and Comprehensive Clinical Management of Oncocytic Thyroid Carcinoma

- Miscellaneous
- COVID-19 Vaccination for Endocrine Patients: A Position Statement from the Korean Endocrine Society
- Cheol Ryong Ku, Kyong Yeun Jung, Chang Ho Ahn, Jun Sung Moon, Ju Hee Lee, Eun Heui Kim, Hyemi Kwon, Hee Kyung Kim, Sunghwan Suh, Sangmo Hong, Jeonghoon Ha, Eun Roh, Jin Hwa Kim, Mi-kyung Kim, the Committee of Clinical Practice Guideline of the Korean Endocrine Society
- Endocrinol Metab. 2021;36(4):757-765. Published online August 17, 2021
- DOI: https://doi.org/10.3803/EnM.2021.404
- 10,360 View
- 419 Download
- 19 Web of Science
- 21 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Since the first outbreak of coronavirus disease 2019 (COVID-19), ongoing efforts have been made to discover an efficacious vaccine against COVID-19 to combat the pandemic. In most countries, both mRNA and DNA vaccines have been administered, and their side effects have also been reported. The clinical course of COVID-19 and the effects of vaccination against COVID-19 are both influenced by patients’ health status and involve a systemic physiological response. In view of the systemic function of endocrine hormones, endocrine disorders themselves and the therapeutics used to treat them can influence the outcomes of vaccination for COVID-19. However, there are very limited data to support the development of clinical guidelines for patients with specific medical backgrounds based on large clinical trials. In the current severe circumstances of the COVID-19 pandemic, position statements made by clinical specialists are essential to provide appropriate recommendations based on both medical evidence and clinical experiences. As endocrinologists, we would like to present the medical background of COVID-19 vaccination, as well as precautions to prevent the side effects of COVID-19 vaccination in patients with specific endocrine disorders, including adrenal insufficiency, diabetes mellitus, osteoporosis, autoimmune thyroid disease, hypogonadism, and pituitary disorders.
-
Citations
Citations to this article as recorded by- COVID-19 mRNA vaccine may trigger subacute thyroiditis
Mehmet Sözen, Ömercan Topaloğlu, Berrin Çetinarslan, Alev Selek, Zeynep Cantürk, Emre Gezer, Damla Köksalan, Taner Bayraktaroğlu
Human Vaccines & Immunotherapeutics.2024; 17(12): 5120. CrossRef - The role of co-morbidities in the development of an AEFI after COVID-19 vaccination in a large prospective cohort with patient-reported outcomes in the Netherlands
C. Ouaddouh, J.W. Duijster, T. Lieber, F.P.A.M. van Hunsel
Expert Opinion on Drug Safety.2024; 23(3): 323. CrossRef - Thyroid dysfunction in COVID-19
David Tak Wai Lui, Chi Ho Lee, Yu Cho Woo, Ivan Fan Ngai Hung, Karen Siu Ling Lam
Nature Reviews Endocrinology.2024;[Epub] CrossRef - Adult-Onset Type 1 Diabetes Development Following COVID-19 mRNA Vaccination
Hyeyeon Moon, Sunghwan Suh, Mi Kyoung Park
Journal of Korean Medical Science.2023;[Epub] CrossRef - Prior immunization status of COVID-19 patients and disease severity: A multicenter retrospective cohort study assessing the different types of immunity
Javaria Aslam, Faisal Shahzad Khan, Muhammad Talha Haris, Hewad Hewadmal, Maryam Khalid, Mohammad Y. Alshahrani, Qurrat-ul-ain Aslam, Irrum Aneela, Urooj Zafar
Vaccine.2023; 41(2): 598. CrossRef - Mortality and Severity of Coronavirus Disease 2019 in Patients with Long-Term Glucocorticoid Therapy: A Korean Nationwide Cohort Study
Eu Jeong Ku, Keeho Song, Kyoung Min Kim, Gi Hyeon Seo, Soon Jib Yoo
Endocrinology and Metabolism.2023; 38(2): 253. CrossRef - Pituitary Diseases and COVID-19 Outcomes in South Korea: A Nationwide Cohort Study
Jeonghoon Ha, Kyoung Min Kim, Dong-Jun Lim, Keeho Song, Gi Hyeon Seo
Journal of Clinical Medicine.2023; 12(14): 4799. CrossRef - Inactivated SARS-CoV-2 vaccination does not disturb the clinical course of Graves’ disease: An observational cohort study
Shichen Xu, Huixin Yu, Xian Cheng, Jing Wu, Jiandong Bao, Li Zhang
Vaccine.2023; 41(38): 5648. CrossRef - Adrenal Crisis Associated With COVID-19 Vaccination in Patients With Adrenal Insufficiency
Yukako Kurematsu, Takako Mohri, Sadanori Okada, Yutaka Takahashi
JCEM Case Reports.2023;[Epub] CrossRef - Adverse Events Associated with COVID-19 Vaccination in Adolescents with Endocrinological Disorders: A Cross-Sectional Study
İbrahim Mert Erbaş, İrem Ceren Erbaş, Gözde Akın Kağızmanlı, Kübra Yüksek Acinikli, Özge Besci, Korcan Demir, Ece Böber, Nurşen Belet, Ayhan Abacı
Journal of Clinical Research in Pediatric Endocrinology.2023; 15(3): 248. CrossRef - Neue Aspekte der Glukokortikoidsubstitution bei Nebennierenrindeninsuffizienz
Tina Kienitz, Gesine Meyer
Der Internist.2022; 63(1): 12. CrossRef - Endocrine Follow-up During Post-Acute COVID-19: Practical Recommendations Based on Available Clinical Evidence
Rimesh Pal, Ameya Joshi, Sanjay K. Bhadada, Mainak Banerjee, Suresh Vaikkakara, Satinath Mukhopadhyay
Endocrine Practice.2022; 28(4): 425. CrossRef - Safety of Inactivated and mRNA COVID-19 Vaccination Among Patients Treated for Hypothyroidism: A Population-Based Cohort Study
Xi Xiong, Carlos King Ho Wong, Ivan Chi Ho Au, Francisco Tsz Tsun Lai, Xue Li, Eric Yuk Fai Wan, Celine Sze Ling Chui, Esther Wai Yin Chan, Franco Wing Tak Cheng, Kristy Tsz Kwan Lau, Chi Ho Lee, Yu Cho Woo, David Tak Wai Lui, Ian Chi Kei Wong
Thyroid.2022; 32(5): 505. CrossRef - The New Entity of Subacute Thyroiditis amid the COVID-19 Pandemic: From Infection to Vaccine
Mihaela Popescu, Adina Ghemigian, Corina Maria Vasile, Andrei Costache, Mara Carsote, Alice Elena Ghenea
Diagnostics.2022; 12(4): 960. CrossRef - Adrenal Crisis Secondary to COVID-19 Vaccination in a Patient With Hypopituitarism
Nikolina Markovic, Anila Faizan, Chirag Boradia, Sridhar Nambi
AACE Clinical Case Reports.2022; 8(4): 171. CrossRef - The Effect of Inactivated SARS-CoV-2 Vaccines on TRAB in Graves’ Disease
LingHong Huang, ZhengRong Jiang, JingXiong Zhou, YuPing Chen, HuiBin Huang
Frontiers in Endocrinology.2022;[Epub] CrossRef - Osteoporosis in Patients With Respiratory Diseases
Yue Ma, Shui Qiu, Renyi Zhou
Frontiers in Physiology.2022;[Epub] CrossRef - Pilot Findings on SARS-CoV-2 Vaccine-Induced Pituitary Diseases: A Mini Review from Diagnosis to Pathophysiology
Ach Taieb, El Euch Mounira
Vaccines.2022; 10(12): 2004. CrossRef - Forty Years Together, New Leap Forward! The 40th Anniversary of the Korean Endocrine Society
Jong Chul Won, Ki-Hyun Baek
Endocrinology and Metabolism.2022; 37(6): 851. CrossRef - No need of glucocorticoid dose adjustment in patients with adrenal insufficiency before COVID-19 vaccine
Tania Pilli, Cristina Dalmiglio, Gilda Dalmazio, Alfonso Sagnella, Raffaella Forleo, Lucia Brilli, Fabio Maino, Cristina Ciuoli, Maria Grazia Castagna
European Journal of Endocrinology.2022; 187(1): K7. CrossRef - Diabetes and COVID-19 Vaccination
Hae Dong Choi, Jun Sung Moon
The Journal of Korean Diabetes.2021; 22(4): 221. CrossRef
- COVID-19 mRNA vaccine may trigger subacute thyroiditis

- Thyroid
- Programmed Cell Death-Ligand 1 (PD-L1) gene Single Nucleotide Polymorphism in Graves’ Disease and Hashimoto’s Thyroiditis in Korean Patients
- Jee Hee Yoon, Min-ho Shin, Hee Nam Kim, Wonsuk Choi, Ji Yong Park, A Ram Hong, Hee Kyung Kim, Ho-Cheol Kang
- Endocrinol Metab. 2021;36(3):599-606. Published online June 2, 2021
- DOI: https://doi.org/10.3803/EnM.2021.965
- 3,998 View
- 117 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Programmed cell death-ligand 1 (PD-L1) has an important role in regulating immune reactions by binding to programmed death 1 (PD-1) on immune cells, which could prevent the exacerbation of autoimmune thyroid disease (AITD). The aim of this study was to evaluate the association of PD-L1 polymorphism with AITD, including Graves’ disease (GD) and Hashimoto’s thyroiditis (HT).
Methods
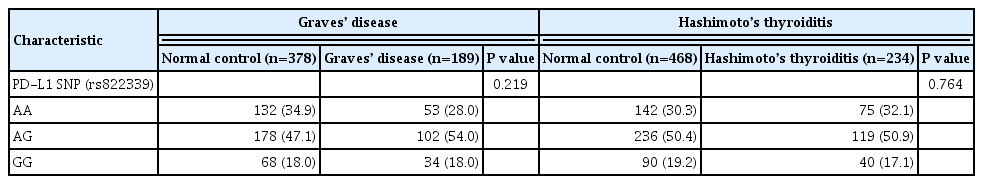
A total of 189 GD patients, 234 HT patients, and 846 healthy age- and sex-matched controls were enrolled in this study. We analyzed PD-L1 single nucleotide polymorphism (SNP) (rs822339) and investigated the associations with clinical disease course and outcome.
Results
Genotype frequency at the PD-L1 marker RS822339 in GD (P=0.219) and HT (P=0.764) patients did not differ from that among healthy controls. In patients with GD, the A/G or G/G genotype group demonstrated higher TBII titer (20.6±20.5 vs. 28.0± 25.8, P=0.044) and longer treatment duration (39.0±40.4 months vs. 62.4±65.0 months, P=0.003) compared to the A/A genotype group. Among patients in whom anti-thyroid peroxidase (TPO) antibody was measured after treatment of GD, post-treatment antiTPO positivity was higher in the A/G or G/G genotype group compared to the A/A genotype group (48.1% vs. 69.9%, P=0.045). Among patients with HT, there was no significant difference of anti-TPO antibody positivity (79.4% vs. 68.6%, P=0.121), anti-thyroglobulin antibody positivity (80.9% vs. 84.7%, P=0.661), or development to overt hypothyroidism (68.0% vs. 71.1%, P=0.632) between the A/A genotype group and the A/G or G/G genotype group.
Conclusion
The genotype frequency of PD-L1 (rs822339) is not different in patients with AITD compared with healthy controls. The intact PD-1/PD-L1 pathway in GD and HT might be important to maintain chronicity of AITD by protecting immune tolerance. However, the PD-L1 SNP could be associated with difficulty in achieving remission in patients with GD, which may be helpful to predict the possibility of longer treatment. Further studies are required to investigate the complex immune tolerance system in patients with AITD. -
Citations
Citations to this article as recorded by- Synergistic effects of BTN3A1, SHP2, CD274, and STAT3 gene polymorphisms on the risk of systemic lupus erythematosus: a multifactorial dimensional reduction analysis
Yang-Yang Tang, Wang-Dong Xu, Lu Fu, Xiao-Yan Liu, An-Fang Huang
Clinical Rheumatology.2024; 43(1): 489. CrossRef - Relationship between CD274 gene polymorphism and systemic lupus erythematosus risk in a Chinese Han population
Lu‐Qi Yang, Zhen Qin, Lu Fu, Wang‐Dong Xu
International Journal of Rheumatic Diseases.2024;[Epub] CrossRef
- Synergistic effects of BTN3A1, SHP2, CD274, and STAT3 gene polymorphisms on the risk of systemic lupus erythematosus: a multifactorial dimensional reduction analysis

- Clinical Study
- Characteristics of Immune-Related Thyroid Adverse Events in Patients Treated with PD-1/PD-L1 Inhibitors
- Jee Hee Yoon, A Ram Hong, Hee Kyung Kim, Ho-Cheol Kang
- Endocrinol Metab. 2021;36(2):413-423. Published online April 6, 2021
- DOI: https://doi.org/10.3803/EnM.2020.906

- 5,641 View
- 218 Download
- 23 Web of Science
- 22 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Thyroid immune-related adverse events (IRAEs) have been reported in patients treated with programmed cell death protein-1 (PD-1) and programmed cell death protein-ligand 1 (PD-L1) inhibitors. We investigated the incidence and clinical course of PD-1/PD-L1 inhibitor-induced thyroid IRAEs, and identified predictable clinical risk factors of thyroid IRAEs, in particular, overt hypothyroidism (OH).
Methods
We retrospectively reviewed the medical records of 325 cancer patients receiving PD-1/PD-L1 inhibitor in a tertiary referral center.
Results
A total of 50.5% (164/325) of patients experienced at least one abnormal thyroid function following PD-1/PD-L1 inhibitor. Eighty-four patients (51.2%) of them recovered to normal thyroid function during follow-up. In overall population, 25 patients (7.7%) required thyroid hormone replacement therapy due to PD-1/PD-L1 inhibitor-induced OH. Patients who progressed to OH showed significantly higher baseline thyroid stimulating hormone level and longer duration of PD-1/PD-L1 inhibitor therapy than those without thyroid dysfunction or OH (both P<0.001). Median time interval to the development of OH was 3 months after the therapy. OH was significantly associated with positive anti-thyroid peroxidase antibody at baseline and anti-thyroglobulin antibody during the therapy than those without thyroid dysfunction or OH (P=0.015 and P=0.005, respectively). We observed no patients with OH who were able to stop levothyroxine replacement after the cessation of PD-1/PD-L1 inhibitor therapy.
Conclusion
PD-1/PD-L1 inhibitor-induced thyroid dysfunctions are considerably reversible; however, OH is irreversible requiring levothyroxine replacement even after stopping the therapy. Positive thyroid autoantibodies may predict the progression to OH. -
Citations
Citations to this article as recorded by- Thyroid Dysfunction after Atezolizumab and Bevacizumab Is Associated with Favorable Outcomes in Hepatocellular Carcinoma
Young Shin Song, Hannah Yang, Beodeul Kang, Jaekyung Cheon, Ilhwan Kim, Hyeyeong Kim, Won Suk Lee, Yun Beom Sang, Sanghoon Jung, Ho Yeong Lim, Vincent E. Gaillard, Chan Kim, Hong Jae Chon
Liver Cancer.2024; 13(1): 89. CrossRef - Thyroid dysfunction (TD) induced by PD-1/PD-L1 inhibitors in advanced lung cancer
Yanling Wang, Xiaoxuan Yang, Jia Ma, Shenglan Chen, Ping Gong, Ping Dai
Heliyon.2024; 10(5): e27077. CrossRef - Non-Invasive Predictive Biomarkers for Immune-Related Adverse Events Due to Immune Checkpoint Inhibitors
Ben Ponvilawan, Abdul Wali Khan, Janakiraman Subramanian, Dhruv Bansal
Cancers.2024; 16(6): 1225. CrossRef - Implication of the Gut Microbiome and Microbial-Derived Metabolites in Immune-Related Adverse Events: Emergence of Novel Biomarkers for Cancer Immunotherapy
David Dora, Syeda Mahak Zahra Bokhari, Kenan Aloss, Peter Takacs, Juliane Zsuzsanna Desnoix, György Szklenárik, Patrick Deniz Hurley, Zoltan Lohinai
International Journal of Molecular Sciences.2023; 24(3): 2769. CrossRef - Immune checkpoint inhibitor-associated toxicity in advanced non-small cell lung cancer: An updated understanding of risk factors
Xiangxiao Hu, Lina Wang, Bin Shang, Junren Wang, Jian Sun, Bin Liang, Lili Su, Wenjie You, Shujuan Jiang
Frontiers in Immunology.2023;[Epub] CrossRef - Immune-related adverse events induced by programmed death protein-1 inhibitors from the perspective of lymphoma immunotherapy
Yong-Zhe Hou, Qin Zhang, Hai Bai, Tao Wu, Ya-Jie Chen
World Journal of Clinical Cases.2023; 11(7): 1458. CrossRef - Predictive Biomarkers for Checkpoint Inhibitor Immune-Related Adverse Events
Iñigo Les, Mireia Martínez, Inés Pérez-Francisco, María Cabero, Lucía Teijeira, Virginia Arrazubi, Nuria Torrego, Ana Campillo-Calatayud, Iñaki Elejalde, Grazyna Kochan, David Escors
Cancers.2023; 15(5): 1629. CrossRef - Immune-related thyroid dysfunctions during anti PD-1/PD-L1 inhibitors: new evidence from a single centre experience
Alice Nervo, Matteo Ferrari, Giovanni Gruosso, Enrica Migliore, Sara Basile, Valentina D’Angelo, Anna Roux, Alessandro Piovesan, Emanuela Arvat
Clinical and Experimental Medicine.2023; 23(8): 4817. CrossRef - RNA Sequencing Reveals Unique Transcriptomic Signatures of the Thyroid in a Murine Lung Cancer Model Treated with PD-1 and PD-L1 Antibodies
Rena Pollack, Joshua Stokar, Natan Lishinsky, Irina Gurt, Naomi Kaisar-Iluz, Merav E. Shaul, Zvi G. Fridlender, Rivka Dresner-Pollak
International Journal of Molecular Sciences.2023; 24(13): 10526. CrossRef - Immune‐related adverse events after immune check point inhibitors: Understanding the intersection with autoimmunity
Namrata Singh, Anne M. Hocking, Jane H. Buckner
Immunological Reviews.2023; 318(1): 81. CrossRef - Endocrine Side Effects in Patients Treated with Immune Checkpoint Inhibitors: A Narrative Review
Nicia I. Profili, Roberto Castelli, Antonio Gidaro, Alessandro Merella, Roberto Manetti, Giuseppe Palmieri, Margherita Maioli, Alessandro P. Delitala
Journal of Clinical Medicine.2023; 12(15): 5161. CrossRef - Incidence of Endocrine-Related Dysfunction in Patients Treated with New Immune Checkpoint Inhibitors: A Meta-Analysis and Comprehensive Review
Won Sang Yoo, Eu Jeong Ku, Eun Kyung Lee, Hwa Young Ahn
Endocrinology and Metabolism.2023; 38(6): 750. CrossRef - PD-1/PD-L1 Inhibitors in Patients With Preexisting Autoimmune Diseases
Ke Zhang, Xiangyi Kong, Yuan Li, Zhongzhao Wang, Lin Zhang, Lixue Xuan
Frontiers in Pharmacology.2022;[Epub] CrossRef - Association between the type of thyroid dysfunction induced by immune checkpoint inhibitors and prognosis in cancer patients
Han-sang Baek, Chaiho Jeong, Kabsoo Shin, Jaejun Lee, Heysun Suh, Dong-Jun Lim, Moo Il Kang, Jeonghoon Ha
BMC Endocrine Disorders.2022;[Epub] CrossRef - A Successful Case of Hepatocellular Carcinoma Treated with Atezolizumab Plus Bevacizumab with Multisystem Immune-related Adverse Events
Hidemi Hayashi, Koji Sawada, Takumu Hasebe, Shunsuke Nakajima, Jun Sawada, Yuri Takiyama, Yumi Takiyama, Toshikatsu Okumura, Mikihiro Fujiya
Internal Medicine.2022; 61(23): 3497. CrossRef - Immune Related Adverse Events of the Thyroid – A Narrative Review
Christopher A. Muir, Venessa H. M. Tsang, Alexander M. Menzies, Roderick J. Clifton-Bligh
Frontiers in Endocrinology.2022;[Epub] CrossRef - Thyroid-related adverse events induced by immune checkpoint inhibitors
Alexandra Chera, Andreea Lucia Stancu, Octavian Bucur
Frontiers in Endocrinology.2022;[Epub] CrossRef - Risk Factors and Biomarkers for Immune-Related Adverse Events: A Practical Guide to Identifying High-Risk Patients and Rechallenging Immune Checkpoint Inhibitors
Adithya Chennamadhavuni, Laith Abushahin, Ning Jin, Carolyn J. Presley, Ashish Manne
Frontiers in Immunology.2022;[Epub] CrossRef - Case 5: A 41-Year-Old Woman With Palpitation
Jiwon Yang, Kabsoo Shin, Jeongmin Lee, Jeonghoon Ha, Dong-Jun Lim, Han-Sang Baek
Journal of Korean Medical Science.2022;[Epub] CrossRef - Immune Checkpoint Inhibitors and Endocrine Disorders: A Position Statement from the Korean Endocrine Society
Hyemi Kwon, Eun Roh, Chang Ho Ahn, Hee Kyung Kim, Cheol Ryong Ku, Kyong Yeun Jung, Ju Hee Lee, Eun Heui Kim, Sunghwan Suh, Sangmo Hong, Jeonghoon Ha, Jun Sung Moon, Jin Hwa Kim, Mi-kyung Kim
Endocrinology and Metabolism.2022; 37(6): 839. CrossRef - Management of Endocrine and Metabolic Toxicities of Immune-Checkpoint Inhibitors: From Clinical Studies to a Real-Life Scenario
Calogera Claudia Spagnolo, Giuseppe Giuffrida, Salvatore Cannavò, Tindara Franchina, Nicola Silvestris, Rosaria Maddalena Ruggeri, Mariacarmela Santarpia
Cancers.2022; 15(1): 246. CrossRef - Antineoplastics
Reactions Weekly.2021; 1874(1): 31. CrossRef
- Thyroid Dysfunction after Atezolizumab and Bevacizumab Is Associated with Favorable Outcomes in Hepatocellular Carcinoma

- Clinical Study
- Clinical Implication of World Health Organization Classification in Patients with Follicular Thyroid Carcinoma in South Korea: A Multicenter Cohort Study
- Meihua Jin, Eun Sook Kim, Bo Hyun Kim, Hee Kyung Kim, Hyon-Seung Yi, Min Ji Jeon, Tae Yong Kim, Ho-Cheol Kang, Won Bae Kim, Young Kee Shong, Mijin Kim, Won Gu Kim
- Endocrinol Metab. 2020;35(3):618-627. Published online September 22, 2020
- DOI: https://doi.org/10.3803/EnM.2020.742
- 5,399 View
- 121 Download
- 8 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
The study aimed to compare the prognostic value of the 4th edition of World Health Organization classification (WHO-2017) with the previous WHO classification (WHO-2004) for follicular thyroid carcinoma (FTC).
Methods
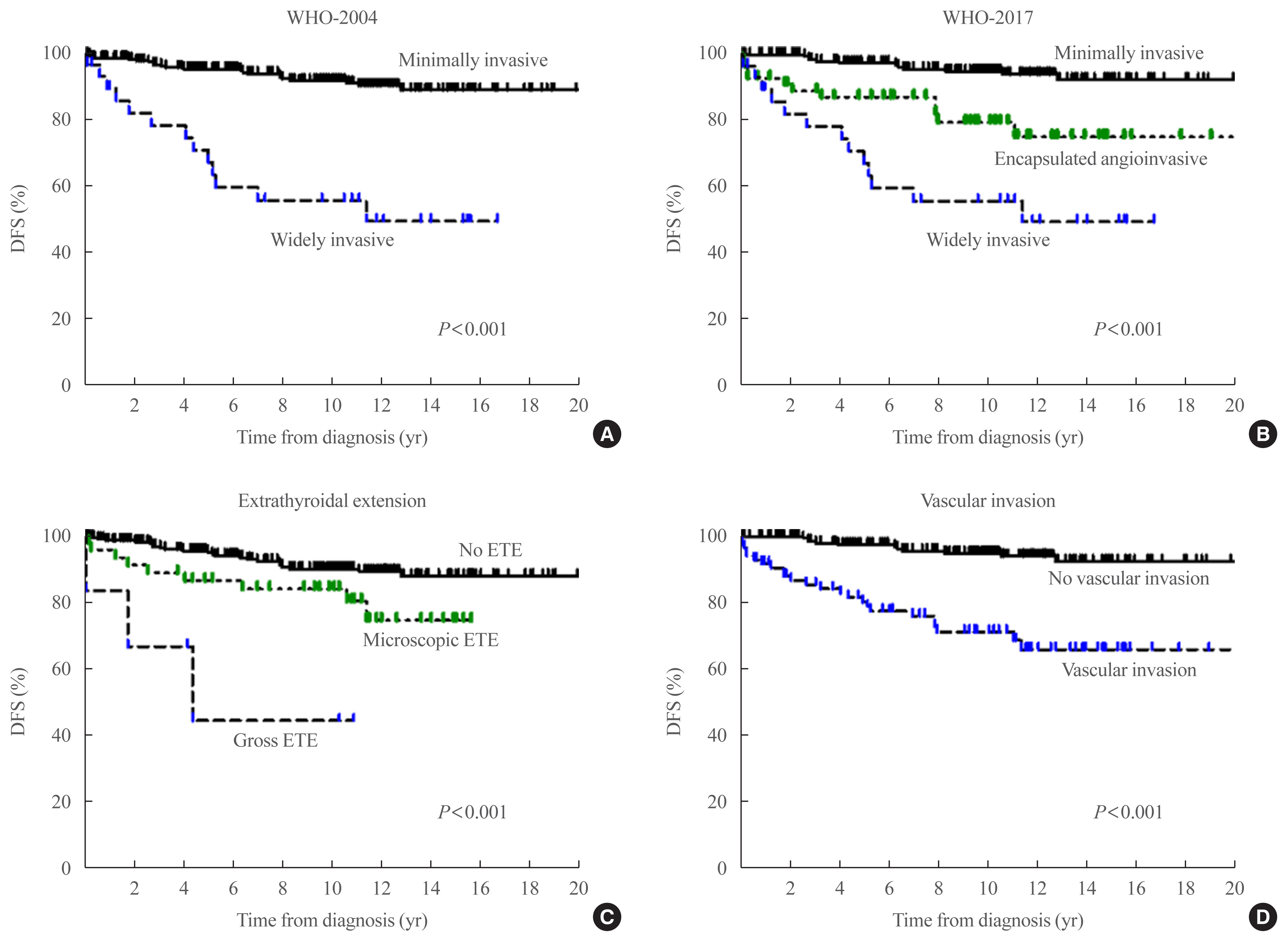
This multicenter retrospective cohort study included 318 patients with FTC from five tertiary centers who underwent thyroid surgery between 1996 and 2009. We evaluated the prognosis of patients with minimally invasive (MI), encapsulated angioinvasive (EA), and widely invasive (WI) FTC according to WHO-2017. Further, we evaluated the proportion of variation explained (PVE) and Harrell’s C-index to compare the predictability of disease-free survival (DFS) and disease-specific survival (DSS).
Results
In total, 227, 58, and 33 patients had MI-, EA-, and WI-FTC, respectively. During a median follow-up of 10.6 years, 46 (14.5%) patients had disease recurrence and 20 (6.3%) patients died from FTC. The 10-year DFS rates of patients with MI-, EA-, and WI-FTC were 91.1%, 78.2%, and 54.9%, respectively (P<0.001, PVE=7.1%, C-index=0.649). The corresponding 10-year DSS rates were 95.9%, 93.5%, and 73.5%, respectively (P<0.001, PVE=2.6%, C-index=0.624). The PVE and C-index values were higher using WHO-2017 than using WHO-2004 for the prediction of DFS, but not for DSS. In multivariate analysis, older age (P=0.02), gross extrathyroidal extension (ETE) (P=0.003), and distant metastasis (P<0.001) were independent risk factors for DSS.
Conclusion
WHO-2017 improves the predictability of DFS, but not DSS, in patients with FTC. Distant metastasis, gross ETE and older age (≥55 years) were independent risk factors for DSS. -
Citations
Citations to this article as recorded by- Association of Ultrasonography Features of Follicular Thyroid Carcinoma With Tumor Invasiveness and Prognosis Based on WHO Classification and TERT Promoter Mutation
Myoung Kyoung Kim, Hyunju Park, Young Lyun Oh, Jung Hee Shin, Tae Hyuk Kim, Soo Yeon Hahn
Korean Journal of Radiology.2024; 25(1): 103. CrossRef - Clinical Outcomes and Implications of Radioactive Iodine Therapy on Cancer-specific Survival in WHO Classification of FTC
Genpeng Li, Ziyang Ye, Tao Wei, Jingqiang Zhu, Zhihui Li, Jianyong Lei
The Journal of Clinical Endocrinology & Metabolism.2024;[Epub] CrossRef - Radioiodine whole body scan pitfalls in differentiated thyroid cancer
Cristina Basso, Alessandra Colapinto, Valentina Vicennati, Alessandra Gambineri, Carla Pelusi, Guido Di Dalmazi, Elisa Lodi Rizzini, Elena Tabacchi, Arber Golemi, Letizia Calderoni, Stefano Fanti, Uberto Pagotto, Andrea Repaci
Endocrine.2024;[Epub] CrossRef - The Prognostic Impact of Extent of Vascular Invasion in Follicular Thyroid Carcinoma
David Leong, Anthony J. Gill, John Turchini, Michael Waller, Roderick Clifton‐Bligh, Anthony Glover, Mark Sywak, Stan Sidhu
World Journal of Surgery.2023; 47(2): 412. CrossRef - TERT Promoter Mutation as a Prognostic Marker in Encapsulated Angioinvasive and Widely Invasive Follicular Thyroid Carcinomas
Yasuhiro Ito, Takashi Akamizu
Clinical Thyroidology.2023; 35(5): 202. CrossRef - Risk factors for death of follicular thyroid carcinoma: a systematic review and meta-analysis
Ting Zhang, Liang He, Zhihong Wang, Wenwu Dong, Wei Sun, Ping Zhang, Hao Zhang
Endocrine.2023; 82(3): 457. CrossRef - Molecular classification of follicular thyroid carcinoma based on TERT promoter mutations
Hyunju Park, Hyeong Chan Shin, Heera Yang, Jung Heo, Chang-Seok Ki, Hye Seung Kim, Jung-Han Kim, Soo Yeon Hahn, Yun Jae Chung, Sun Wook Kim, Jae Hoon Chung, Young Lyun Oh, Tae Hyuk Kim
Modern Pathology.2022; 35(2): 186. CrossRef - Whole-genome Sequencing of Follicular Thyroid Carcinomas Reveal Recurrent Mutations in MicroRNA Processing Subunit DGCR8
Johan O Paulsson, Nima Rafati, Sebastian DiLorenzo, Yi Chen, Felix Haglund, Jan Zedenius, C Christofer Juhlin
The Journal of Clinical Endocrinology & Metabolism.2021; 106(11): 3265. CrossRef - Clinicopathological Characteristics and Disease-Free Survival in Patients with Hürthle Cell Carcinoma: A Multicenter Cohort Study in South Korea
Meihua Jin, Eun Sook Kim, Bo Hyun Kim, Hee Kyung Kim, Yea Eun Kang, Min Ji Jeon, Tae Yong Kim, Ho-Cheol Kang, Won Bae Kim, Young Kee Shong, Mijin Kim, Won Gu Kim
Endocrinology and Metabolism.2021; 36(5): 1078. CrossRef
- Association of Ultrasonography Features of Follicular Thyroid Carcinoma With Tumor Invasiveness and Prognosis Based on WHO Classification and TERT Promoter Mutation

- Clinical Study
- Vandetanib for the Management of Advanced Medullary Thyroid Cancer: A Real-World Multicenter Experience
- Mijin Kim, Jee Hee Yoon, Jonghwa Ahn, Min Ji Jeon, Hee Kyung Kim, Dong Jun Lim, Ho-Cheol Kang, In Joo Kim, Young Kee Shong, Tae Yong Kim, Bo Hyun Kim
- Endocrinol Metab. 2020;35(3):587-594. Published online September 22, 2020
- DOI: https://doi.org/10.3803/EnM.2020.687
- 5,626 View
- 146 Download
- 12 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
Vandetanib is the most widely used tyrosine kinase inhibitor for the treatment of patients with advanced medullary thyroid cancer (MTC). However, only limited data regarding its use outside clinical trials are available. We aimed to evaluate the efficacy and safety of vandetanib in patients with advanced MTC in routine clinical practice.
Methods
In this multicenter retrospective study, 12 patients with locally advanced or metastatic MTC treated with vandetanib at four tertiary hospitals were included. The primary outcome was the objective response rate (ORR) based on the Response Evaluation Criteria in Solid Tumors. The progression-free survival (PFS), overall survival (OS), and toxicities were also evaluated.
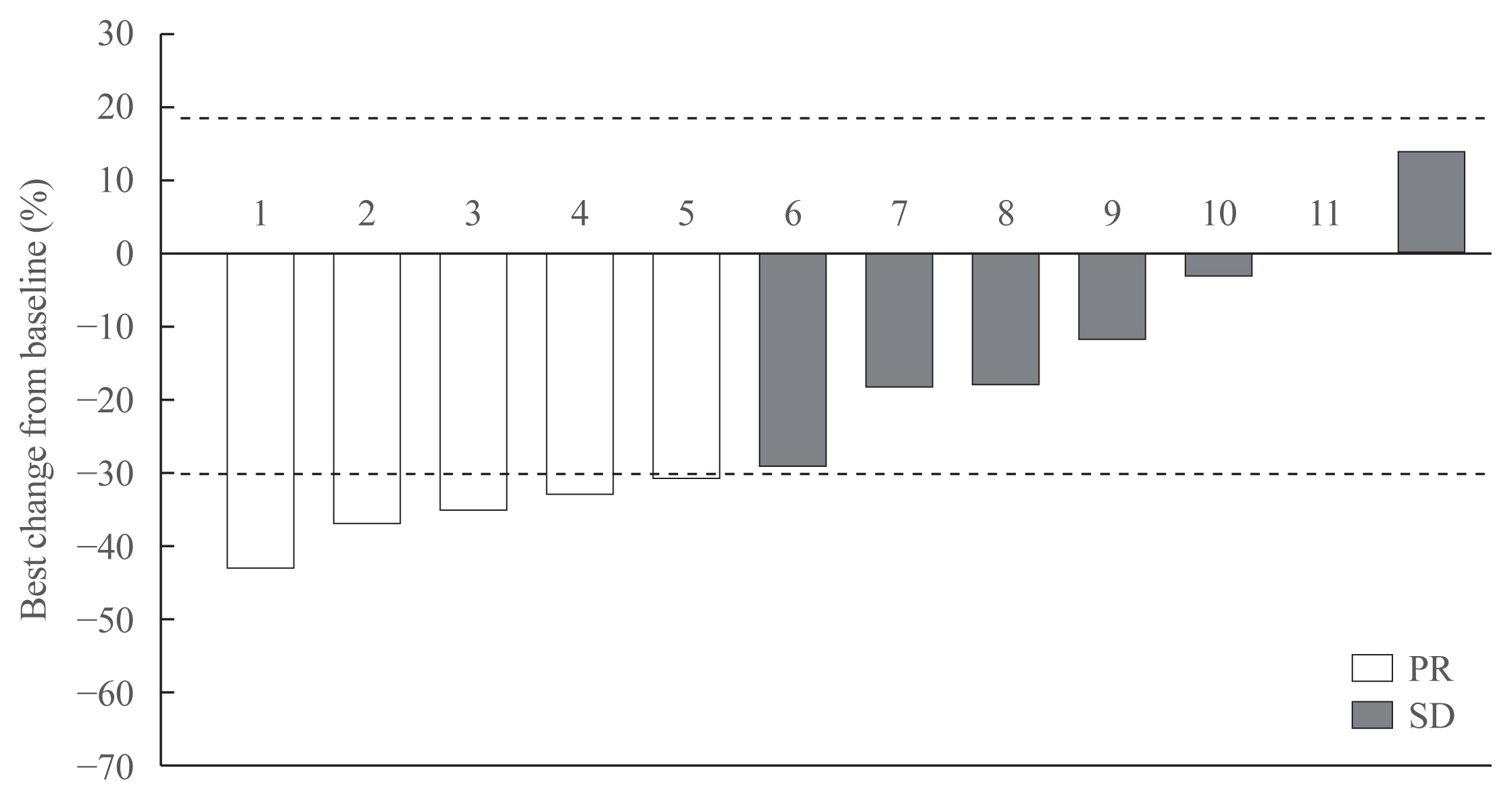
Results
Eleven patients (92%) had distant metastasis and 10 (83%) had disease progression at enrollment. Partial response was observed in five patients (ORR, 42%) and stable disease lasting ≥24 weeks was reported in an additional five patients (83%). During the median 31.7 months of follow-up, disease progression was seen in five patients (42%); of these, two died due to disease progression. The median PFS was 25.9 months, while the median OS was not reached. All patients experienced adverse events (AEs) which were generally consistent with the known safety profile of vandetanib. Vandetanib was discontinued in two patients due to skin toxicity.
Conclusion
Consistent with the phase III trial, this study confirmed the efficacy of vandetanib for advanced MTC in terms of both ORR and PFS in the real-world setting. Vandetanib was well tolerated in the majority of patients, and there were no fatal AEs. -
Citations
Citations to this article as recorded by- Metastatic medullary thyroid carcinoma (MTC): disease course, treatment modalities and factors predisposing for drug resistance
Katerina Saltiki, George Simeakis, Olga Karapanou, Stavroula A. Paschou, Maria Alevizaki
Endocrine.2023; 80(3): 570. CrossRef - Initial Experiences of Selective RET Inhibitor Selpercatinib in Adults with Metastatic Differentiated Thyroid Carcinoma and Medullary Thyroid Carcinoma: Real-World Case Series in Korea
Han-Sang Baek, Jeonghoon Ha, Seunggyun Ha, Ja Seong Bae, Chan Kwon Jung, Dong-Jun Lim
Current Oncology.2023; 30(3): 3020. CrossRef - Molecular Basis and Natural History of Medullary Thyroid Cancer: It is (Almost) All in the RET
Nicolas Sahakian, Frédéric Castinetti, Pauline Romanet
Cancers.2023; 15(19): 4865. CrossRef - Sporadic Medullary Thyroid Carcinoma: Towards a Precision Medicine
Antonio Matrone, Carla Gambale, Alessandro Prete, Rossella Elisei
Frontiers in Endocrinology.2022;[Epub] CrossRef - Targeted therapy and drug resistance in thyroid cancer
Yujie Zhang, Zhichao Xing, Tianyou Liu, Minghai Tang, Li Mi, Jingqiang Zhu, Wenshuang Wu, Tao Wei
European Journal of Medicinal Chemistry.2022; 238: 114500. CrossRef - Daily Management of Patients on Multikinase Inhibitors’ Treatment
Carla Colombo, Simone De Leo, Matteo Trevisan, Noemi Giancola, Anna Scaltrito, Laura Fugazzola
Frontiers in Oncology.2022;[Epub] CrossRef - The Angiogenic Balance and Its Implications in Cancer and Cardiovascular Diseases: An Overview
Cătălina Ionescu, Bogdan Oprea, Georgeta Ciobanu, Milena Georgescu, Ramona Bică, Garofiţa-Olivia Mateescu, Fidan Huseynova, Veronique Barragan-Montero
Medicina.2022; 58(7): 903. CrossRef - Reassessing vascular endothelial growth factor (VEGF) in anti-angiogenic cancer therapy
Tobiloba C. Elebiyo, Damilare Rotimi, Ikponmwosa O. Evbuomwan, Rotdelmwa Filibus Maimako, Matthew Iyobhebhe, Oluwafemi Adeleke Ojo, Olarewaju M. Oluba, Oluyomi S. Adeyemi
Cancer Treatment and Research Communications.2022; 32: 100620. CrossRef - Current Guidelines for Management of Medullary Thyroid Carcinoma
Mijin Kim, Bo Hyun Kim
Endocrinology and Metabolism.2021; 36(3): 514. CrossRef - Recent advances in precision medicine for the treatment of medullary thyroid cancer
Jolanta Krajewska, Aleksandra Kukulska, Malgorzata Oczko-Wojciechowska, Barbara Jarzab
Expert Review of Precision Medicine and Drug Development.2021; 6(5): 307. CrossRef - Functional evaluation of vandetanib metabolism by CYP3A4 variants and potential drug interactions in vitro
Mingming Han, Xiaodan Zhang, Zhize Ye, Jing Wang, Jianchang Qian, Guoxin Hu, Jianping Cai
Chemico-Biological Interactions.2021; 350: 109700. CrossRef - Nephrotoxicity in advanced thyroid cancer treated with tyrosine kinase inhibitors: An update
Alice Nervo, Francesca Retta, Alberto Ragni, Alessandro Piovesan, Alberto Mella, Luigi Biancone, Marco Manganaro, Marco Gallo, Emanuela Arvat
Critical Reviews in Oncology/Hematology.2021; 168: 103533. CrossRef
- Metastatic medullary thyroid carcinoma (MTC): disease course, treatment modalities and factors predisposing for drug resistance

- Clinical Study
- Modification of the Tumor-Node-Metastasis Staging System for Differentiated Thyroid Carcinoma by Considering Extra-Thyroidal Extension and Lateral Cervical Lymph Node Metastasis
- Mijin Kim, Won Gu Kim, Min Ji Jeon, Hee Kyung Kim, Hyon-Seung Yi, Eun Sook Kim, Bo Hyun Kim, Won Bae Kim, Young Kee Shong, Ho-Cheol Kang, Tae Yong Kim
- Endocrinol Metab. 2020;35(1):149-156. Published online March 19, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.1.149
- 5,242 View
- 82 Download
- 6 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
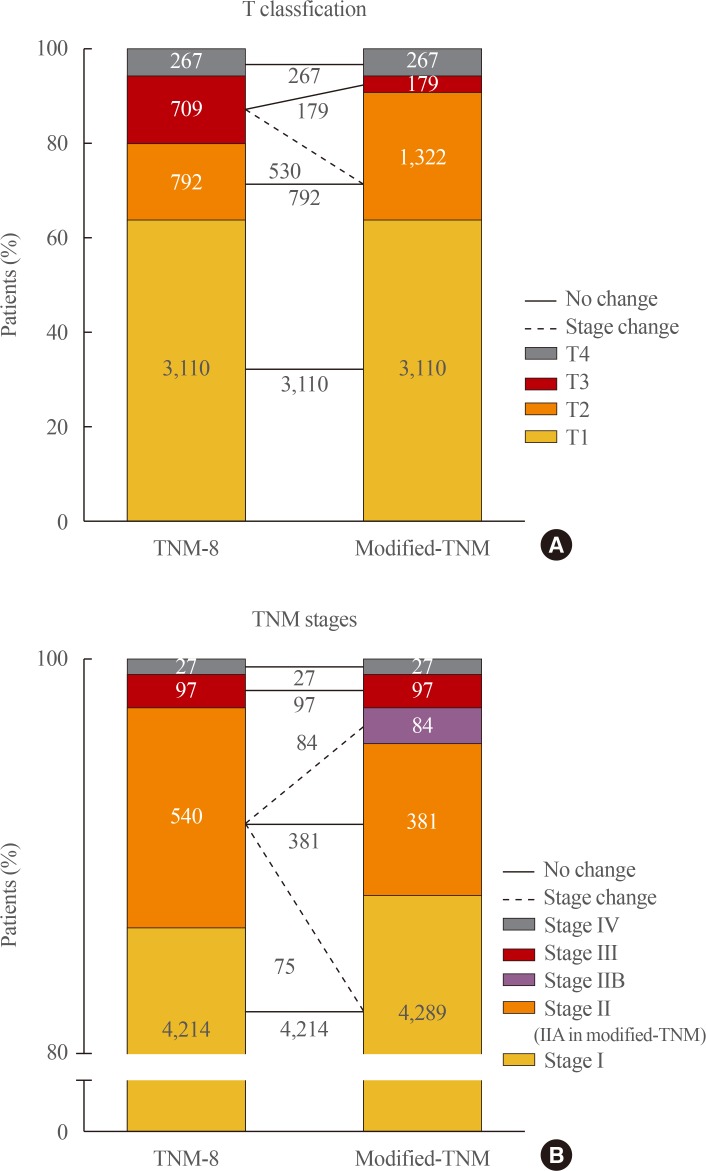
ePub Background Concerns have arisen about the classification of extra-thyroidal extension (ETE) and lateral cervical lymph node metastasis (N1b) in the 8th edition of the tumor-node-metastasis staging system (TNM-8). This study evaluated the prognostic validity of a modified-TNM staging system, focusing on ETE and N1b, in differentiated thyroid carcinoma (DTC) patients.
Methods This multicenter retrospective cohort study included 4,878 DTC patients from five tertiary hospitals. In the modified-TNM, T3b in TNM-8 was down-staged to T2, and stage II was subdivided into stages IIA and IIB. Older patients with N1b were reclassified as stage IIB.
Results The modified-TNM resulted in staging migration in 540 patients (11%) classified as stage II according to the TNM-8, with 75 (14%), 381 (71%), and 84 patients (16%) classified as stages I, IIA, and IIB, respectively. The 10-year disease-specific survival (DSS) rates in patients classified as stages I, II, III, and IV by TNM-8 were 99.8%, 95.9%, 81.0%, and 41.6%, respectively. The DSS rates of patients classified as stages I, IIA, IIB, III, and IV according to the modified-TNM were 99.8%, 96.4%, 93.3%, 81.0%, and 41.6%, respectively. DSS curves between stages on TNM-8 (
P <0.001) and modified-TNM (P <0.001) differed significantly, but the modified-TNM discriminated better than TNM-8. The proportions of variation explained values of TNM-8 and modified-TNM were 6.3% and 6.5%, respectively.Conclusion Modification of the TNM staging system focusing on ETE and N1b could improve the prediction of DSS in patients with DTC. Further researches are needed to validate the prognostic accuracy of this modified-TNM staging system.
-
Citations
Citations to this article as recorded by- Clinicopathological features of differentiated thyroid carcinoma as predictors of the effects of radioactive iodine therapy
Wen Liu, Beibei Jiang, Jingli Xue, Ruijing Liu, Yuqing Wei, Peifeng Li
Annals of Diagnostic Pathology.2024; 69: 152243. CrossRef - Thyroid Collision Tumors: The Presence of the Medullary Thyroid Carcinoma Component Negatively Influences the Prognosis
Ion Negura, Victor Ianole, Mihai Danciu, Cristina Preda, Diana Gabriela Iosep, Radu Dănilă, Alexandru Grigorovici, Delia Gabriela Ciobanu Apostol
Diagnostics.2023; 13(2): 285. CrossRef - Serum thyroglobulin testing after thyroid lobectomy in patients with 1–4 cm papillary thyroid carcinoma
Ahreum Jang, Meihua Jin, Chae A Kim, Min Ji Jeon, Yu-Mi Lee, Tae-Yon Sung, Tae Yong Kim, Won Bae Kim, Young Kee Shong, Won Gu Kim
Endocrine.2023; 81(2): 290. CrossRef - Prognostic Impact of Microscopic Extra-Thyroidal Extension (mETE) on Disease Free Survival in Patients with Papillary Thyroid Carcinoma (PTC)
Nadia Bouzehouane, Pascal Roy, Myriam Decaussin-Petrucci, Mireille Bertholon-Grégoire, Chantal Bully, Agnès Perrin, Helene Lasolle, Jean-Christophe Lifante, Françoise Borson-Chazot, Claire Bournaud
Cancers.2022; 14(11): 2591. CrossRef - Impacts of the American Joint Committee on Cancer (AJCC) 8th edition tumor, node, metastasis (TNM) staging system on outcomes of differentiated thyroid cancer in Thai patients
Yotsapon Thewjitcharoen, Waralee Chatchomchuan, Krittadhee Karndumri, Sriurai Porramatikul, Sirinate Krittiyawong, Ekgaluck Wanothayaroj, Siriwan Butadej, Soontaree Nakasatien, Veekij Veerasomboonsin, Auchai Kanchanapituk, Rajata Rajatanavin, Thep Himatho
Heliyon.2021; 7(3): e06624. CrossRef
- Clinicopathological features of differentiated thyroid carcinoma as predictors of the effects of radioactive iodine therapy

- Thyroid
- Prognosis of Differentiated Thyroid Carcinoma with Initial Distant Metastasis: A Multicenter Study in Korea
- Hosu Kim, Hye In Kim, Sun Wook Kim, Jaehoon Jung, Min Ji Jeon, Won Gu Kim, Tae Yong Kim, Hee Kyung Kim, Ho-Cheol Kang, Ji Min Han, Yoon Young Cho, Tae Hyuk Kim, Jae Hoon Chung
- Endocrinol Metab. 2018;33(2):287-295. Published online June 21, 2018
- DOI: https://doi.org/10.3803/EnM.2018.33.2.287
- 5,434 View
- 59 Download
- 31 Web of Science
- 28 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Background Most patients with differentiated thyroid cancer (DTC) have a favorable prognosis. However, patients with DTC and initial distant metastasis have not been commonly found, and their clinical characteristics have seldom been reported. In this study, we analyzed the clinical features and prognosis of patients with DTC and initial distant metastasis in Korea.
Methods We retrospectively reviewed the clinical data of 242 patients with DTC and initial distant metastasis treated from 1994 to 2013, collected from five tertiary hospitals in Korea.
Results The patients' median age was 51 years, and 65% were women. They were followed for a median of 7 years. Lung was the most common site of distant metastasis: only lung 149 patients (62%), only bone 49 (20%), other single site one (pleura), and combined sites 43 (40 were lung and bone, two were bone and other site, and one was lung and other site). At the time of diagnosis, 50 patients (21%) had non-radioactive iodine (RAI) avidity. Five-year disease-specific survival (DSS) was 85% and 10-year DSS was 68%, which were better than those in previous studies. After multivariate analysis, old age, male sex, metastatic site, and histologic type (follicular type) were significant factors for poor prognosis. However, negative RAI avidity status was not a significant prognostic factor after adjusting for other variables.
Conclusion The prognosis of Korean patients with DTC and initial distant metastasis was better than in previous studies. Old age, male sex, metastasis site, and histologic type were significant prognostic factors.
-
Citations
Citations to this article as recorded by- Case report: A case of hyperthyroidism secondary to bone metastasis of differentiated thyroid cancer
Tingyu Gu, Zhihong Zhao, Yuanyuan Shi, Zhenhua Sun, Yao Wang, Zhiyuan He, Kun Wang
Frontiers in Oncology.2024;[Epub] CrossRef - Theranostics of Thyroid Cancer
Luca Giovanella, Murat Tuncel, Atena Aghaee, Alfredo Campenni, Armando De Virgilio, Petra Petranović Ovčariček
Seminars in Nuclear Medicine.2024;[Epub] CrossRef - Thyroid Hormone Withdrawal versus Recombinant Human TSH as Preparation for I-131 Therapy in Patients with Metastatic Thyroid Cancer: A Systematic Review and Meta-Analysis
Luca Giovanella, Maria Luisa Garo, Alfredo Campenní, Petra Petranović Ovčariček, Rainer Görges
Cancers.2023; 15(9): 2510. CrossRef - Molecular Theranostics in Radioiodine-Refractory Differentiated Thyroid Cancer
Petra Petranović Ovčariček, Alfredo Campenni, Bart de Keizer, Desiree Deandreis, Michael C. Kreissl, Alexis Vrachimis, Murat Tuncel, Luca Giovanella
Cancers.2023; 15(17): 4290. CrossRef - Differentiating pulmonary metastasis from benign lung nodules in thyroid cancer patients using dual-energy CT parameters
Taeho Ha, Wooil Kim, Jaehyung Cha, Young Hen Lee, Hyung Suk Seo, So Young Park, Nan Hee Kim, Sung Ho Hwang, Hwan Seok Yong, Yu-Whan Oh, Eun-Young Kang, Cherry Kim
European Radiology.2022; 32(3): 1902. CrossRef - Feasibility of Recombinant Human TSH as a Preparation for Radioiodine Therapy in Patients with Distant Metastases from Papillary Thyroid Cancer: Comparison of Long-Term Survival Outcomes with Thyroid Hormone Withdrawal
Hsi-Chen Tsai, Kung-Chu Ho, Shih-Hsin Chen, Jing-Ren Tseng, Lan-Yan Yang, Kun-Ju Lin, Ju-Chin Cheng, Miaw-Jene Liou
Diagnostics.2022; 12(1): 221. CrossRef - Long-Term Quality of Life (5-15 Years Post-Thyroidectomy) of Thyroid Carcinoma Patients in Two Tertiary Care Hospitals
Mohammed Yousef Alyousef, Mohammed Khaled Ghandour, Mohammed Al-Mohawes, Mosaad Alnwaisir, Tahera Islam, Khalid Al Qahtani
Cureus.2022;[Epub] CrossRef - Evaluation of Lipocalin-2 and Twist expression in thyroid cancers and its relationship with epithelial mesenchymal transition
Pınar Celepli, İrem Bigat, Sefika Karabulut, Salih Celepli, Sema Hücümenoğlu
Annals of Diagnostic Pathology.2022; 59: 151973. CrossRef - Clinical study of ultrasonic evaluation of T/N staging of differentiated thyroid carcinoma using AJCC 8th staging criteria
Yu Liang, Xingxiang Huang, Zhe Song, Yang Yang, Ju Lei, Mei Ren, Li Tan, Hui Zhang, Francis Moore
PLOS ONE.2022; 17(6): e0269994. CrossRef - Therapeutic challenges in metastatic follicular thyroid cancer occurring in pregnancy: A case report
Claudio Spinelli, Beatrice Sanna, Marco Ghionzoli, Elisabetta Micelli
World Journal of Obstetrics and Gynecology.2022; 11(3): 33. CrossRef - Initial clinical and treatment patterns of advanced differentiated thyroid cancer: ERUDIT study
Juan Antonio Vallejo Casas, Marcel Sambo, Carlos López López, Manuel Durán-Poveda, Julio Rodríguez-Villanueva García, Rita Joana Santos, Marta Llanos, Elena Navarro-González, Javier Aller, Virginia Pubul, Sonsoles Guadalix, Guillermo Crespo, Cintia Gonzál
European Thyroid Journal.2022;[Epub] CrossRef - Male sex is not an independent risk factor for recurrence of differentiated thyroid cancer: a propensity score-matching study
Joonseon Park, Kwangsoon Kim, Dong-Jun Lim, Ja Seong Bae, Jeong Soo Kim
Scientific Reports.2021;[Epub] CrossRef - Evaluation of the 2015 ATA Guidelines in Patients With Distant Metastatic Differentiated Thyroid Cancer
Evert F S van Velsen, Merel T Stegenga, Folkert J van Kemenade, Boen L R Kam, Tessa M van Ginhoven, W Edward Visser, Robin P Peeters
The Journal of Clinical Endocrinology & Metabolism.2020; 105(3): e457. CrossRef - Usefulness of a 3D‐Printed Thyroid Cancer Phantom for Clinician to Patient Communication
Dayeong Hong, Sangwook Lee, Taehun Kim, Jung Hwan Baek, Won Woong Kim, Ki‐Wook Chung, Namkug Kim, Tae‐Yon Sung
World Journal of Surgery.2020; 44(3): 788. CrossRef - Estimating the Growth Rate of Lung Metastases in Differentiated Thyroid Carcinoma: Response Evaluation Criteria in Solid Tumors or Doubling Time?
Eyun Song, Jonghwa Ahn, Min Ji Jeon, Sang Min Lee, Jeong Hyun Lee, Tae Yong Kim, Jung Hwan Baek, Won Bae Kim, Young Kee Shong, Won Gu Kim
Thyroid.2020; 30(3): 418. CrossRef - Personalized management of differentiated thyroid cancer in real life – practical guidance from a multidisciplinary panel of experts
Alfredo Campennì, Daniele Barbaro, Marco Guzzo, Francesca Capoccetti, Luca Giovanella
Endocrine.2020; 70(2): 280. CrossRef - Unusual metastases from differentiated thyroid cancers: A multicenter study in Korea
Jee Hee Yoon, Min Ji Jeon, Mijin Kim, A. Ram Hong, Hee Kyung Kim, Dong Yeob Shin, Bo Hyun Kim, Won Bae Kim, Young Kee Shong, Ho-Cheol Kang, Domenico Albano
PLOS ONE.2020; 15(8): e0238207. CrossRef - Extended Real-World Observation of Patients Treated with Sorafenib for Radioactive Iodine-Refractory Differentiated Thyroid Carcinoma and Impact of Lenvatinib Salvage Treatment: A Korean Multicenter Study
Hye-Seon Oh, Dong Yeob Shin, Mijin Kim, So Young Park, Tae Hyuk Kim, Bo Hyun Kim, Eui Young Kim, Won Bae Kim, Jae Hoon Chung, Young Kee Shong, Dong Jun Lim, Won Gu Kim
Thyroid.2019; 29(12): 1804. CrossRef - Clinical outcomes and prognostic factors in patients with no less than three distant organ system metastases from differentiated thyroid carcinoma
Xin-Yun Zhang, Jian-Wen Sun, Zhong-Ling Qiu, Yang Wang, Xiao-Yue Chen, Jin-Hua Zhao, Quan-Yong Luo
Endocrine.2019; 66(2): 254. CrossRef - Molecular Profile and Clinical Outcomes in Differentiated Thyroid Cancer Patients Presenting with Bone Metastasis
Nilma Malik, Alyaksandr V. Nikitski, Elie Klam, Jason Hunt, Benjamin Witt, Barbara Chadwick, Yuri E. Nikiforov, Devaprabu Abraham
Endocrine Practice.2019; 25(12): 1255. CrossRef - Improved survival after early detection of asymptomatic distant metastasis in patients with thyroid cancer
Hosu Kim, So Young Park, Jaehoon Jung, Jung-Han Kim, Soo Yeon Hahn, Jung Hee Shin, Young Lyun Oh, Man Ki Chung, Hye In Kim, Sun Wook Kim, Jae Hoon Chung, Tae Hyuk Kim
Scientific Reports.2019;[Epub] CrossRef - Unusual metastases from differentiated thyroid carcinoma: analysis of 36 cases
Anabela Zunino, Fabián Pitoia, Eduardo Faure, Adriana Reyes, Mónica Sala, Rosana Sklate, Verónica Ilera, Inés Califano
Endocrine.2019; 65(3): 630. CrossRef - The Prognosis of Papillary Thyroid Cancer with Initial Distant Metastasis is Strongly Associated with Extensive Extrathyroidal Extension: A Retrospective Cohort Study
Young Ki Lee, Daham Kim, Dong Yeob Shin, Cho Rok Lee, Eun Jig Lee, Sang-Wook Kang, Jandee Lee, Jong Ju Jeong, Kee-Hyun Nam, Woong Youn Chung, Cheong Soo Park
Annals of Surgical Oncology.2019; 26(7): 2200. CrossRef - Risk Factors for Distant Metastasis in Follicular Thyroid Carcinoma in Korea
Shin Dol Jo, Joon-Hyop Lee, Suk Ha Kang, Yun Yeong Kim, Yong Soon Chun, Heung Kyu Park, Sang Tae Choi, Jin Mo Kang, Yoo Seung Chung
Journal of Endocrine Surgery.2019; 19(1): 1. CrossRef - Expression levels of ARHI and Beclin1 in thyroid cancer and their relationship with clinical pathology and prognosis
Houwei Zhu, Yanqing Qu
Oncology Letters.2019;[Epub] CrossRef - 甲状腺腫瘍治療の最新情報
Nippon Jibiinkoka Gakkai Kaiho.2018; 121(11): 1336. CrossRef - Clinical Outcomes of Differentiated Thyroid Cancer Patients with Local Recurrence or Distant Metastasis Detected in Old Age
Ji Min Han, Ji Cheol Bae, Hye In Kim, Sam Kwon, Min Ji Jeon, Won Gu Kim, Tae Yong Kim, Young Kee Shong, Won Bae Kim
Endocrinology and Metabolism.2018; 33(4): 459. CrossRef - Efficacy and Affecting Factors of 131I Thyroid Remnant Ablation After Surgical Treatment of Differentiated Thyroid Carcinoma
Chen Wang, Hongcui Diao, Ping Ren, Xufu Wang, Yangang Wang, Wenjuan Zhao
Frontiers in Oncology.2018;[Epub] CrossRef
- Case report: A case of hyperthyroidism secondary to bone metastasis of differentiated thyroid cancer

- Clinical Study
- Disease-Specific Mortality of Differentiated Thyroid Cancer Patients in Korea: A Multicenter Cohort Study
- Min Ji Jeon, Won Gu Kim, Tae Hyuk Kim, Hee Kyung Kim, Bo Hyun Kim, Hyon-Seung Yi, Eun Sook Kim, Hosu Kim, Young Nam Kim, Eun Heui Kim, Tae Yong Kim, Sun Wook Kim, Ho-Cheol Kang, Jae Hoon Chung, Young Kee Shong, Won Bae Kim
- Endocrinol Metab. 2017;32(4):434-441. Published online November 22, 2017
- DOI: https://doi.org/10.3803/EnM.2017.32.4.434
- 5,785 View
- 53 Download
- 29 Web of Science
- 26 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background Little is known regarding disease-specific mortality of differentiated thyroid cancer (DTC) patients and its risk factors in Korea.
Methods We retrospectively reviewed a large multi-center cohort of thyroid cancer from six Korean hospitals and included 8,058 DTC patients who underwent initial surgery between 1996 and 2005.
Results Mean age of patients at diagnosis was 46.2±12.3 years; 87% were females. Most patients had papillary thyroid cancer (PTC; 97%) and underwent total thyroidectomy (85%). Mean size of the primary tumor was 1.6±1.0 cm. Approximately 40% of patients had cervical lymph node (LN) metastases and 1.3% had synchronous distant metastases. During 11.3 years of follow-up, 150 disease-specific mortalities (1.9%) occurred; the 10-year disease-specific survival (DSS) rate was 98%. According to the year of diagnosis, the number of disease-specific mortality was not different. However, the rate of disease-specific mortality decreased during the study period (from 7.7% to 0.7%). Older age (≥45 years) at diagnosis, male, follicular thyroid cancer (FTC) versus PTC, larger tumor size (>2 cm), presence of extrathyroidal extension (ETE), lateral cervical LN metastasis, distant metastasis and tumor node metastasis (TNM) stage were independent risk factors of disease-specific mortality of DTC patients.
Conclusion The rate of disease-specific mortality of Korean DTC patients was 1.9%; the 10-year DSS rate was 98% during 1996 to 2005. Older age at diagnosis, male, FTC, larger tumor size, presence of ETE, lateral cervical LN metastasis, distant metastasis, and TNM stages were significant risk factors of disease-specific mortality of Korean DTC patients.
-
Citations
Citations to this article as recorded by- Log odds of negative lymph nodes/T stage ratio (LONT): A new prognostic tool for differentiated thyroid cancer without metastases in patients aged 55 and older
Xuezhen Wang, Yufan Wu, Xiaoxia Li, Jinsheng Hong, Mingwei Zhang
Frontiers in Endocrinology.2023;[Epub] CrossRef - The association between vitamin D supplementation and the long-term prognosis of differentiated thyroid cancer patients: a retrospective observational cohort study with propensity score matching
Jong-hyuk Ahn, Hoonsung Choi, Su-jin Kim, Sun Wook Cho, Kyu Eun Lee, Do Joon Park, Young Joo Park
Frontiers in Endocrinology.2023;[Epub] CrossRef - Linear association between radioactive iodine dose and second primary malignancy risk in thyroid cancer
Kyeong Jin Kim, Kyoung Jin Kim, Jimi Choi, Nam Hoon Kim, Sin Gon Kim
JNCI: Journal of the National Cancer Institute.2023; 115(6): 695. CrossRef - Outcomes of Advanced Medullary Thyroid Carcinoma in the Era of Targeted Therapy
Nicholas L. Kesby, Alexander J. Papachristos, Matti Gild, Ahmad Aniss, Mark S. Sywak, Roderick Clifton-Bligh, Stan B. Sidhu, Anthony R. Glover
Annals of Surgical Oncology.2022; 29(1): 64. CrossRef - Clinical Implication of Mutifocality for Risk of Recurrence in Patients With Papillary Thyroid Carcinoma
Kwangsoon Kim, Ja Seong Bae, Jeong Soo Kim
Journal of Endocrine Surgery.2022; 22(1): 10. CrossRef - Clinical Factors Predictive of Lymph Node Metastasis in Thyroid Cancer Patients: A Multivariate Analysis
Hui Zheng, Victoria Lai, Jana Lu, Jin K Kang, Jiling Chou, Kenneth D Burman, Leonard Wartofsky, Jennifer E Rosen
Journal of the American College of Surgeons.2022; 234(4): 691. CrossRef - Minimal extrathyroidal extension is associated with lymph node metastasis in single papillary thyroid microcarcinoma: a retrospective analysis of 814 patients
Ra-Yeong Song, Hee Sung Kim, Kyung Ho Kang
World Journal of Surgical Oncology.2022;[Epub] CrossRef - Central Lymph Node Ratio Predicts Recurrence in Patients with N1b Papillary Thyroid Carcinoma
Il Ku Kang, Kwangsoon Kim, Joonseon Park, Ja Seong Bae, Jeong Soo Kim
Cancers.2022; 14(15): 3677. CrossRef - Characterization of the CpG island methylator phenotype subclass in papillary thyroid carcinoma
Pengfei Gu, Yu Zeng, Weike Ma, Wei Zhang, Yu Liu, Fengli Guo, Xianhui Ruan, Jiadong Chi, Xiangqian Zheng, Ming Gao
Frontiers in Endocrinology.2022;[Epub] CrossRef - MicroRNA Profile for Diagnostic and Prognostic Biomarkers in Thyroid Cancer
Jong-Lyul Park, Seon-Kyu Kim, Sora Jeon, Chan-Kwon Jung, Yong-Sung Kim
Cancers.2021; 13(4): 632. CrossRef - Lactate Dehydrogenase A as a Potential New Biomarker for Thyroid Cancer
Eun Jeong Ban, Daham Kim, Jin Kyong Kim, Sang-Wook Kang, Jandee Lee, Jong Ju Jeong, Kee-Hyun Nam, Woong Youn Chung, Kunhong Kim
Endocrinology and Metabolism.2021; 36(1): 96. CrossRef - Male sex is not an independent risk factor for recurrence of differentiated thyroid cancer: a propensity score-matching study
Joonseon Park, Kwangsoon Kim, Dong-Jun Lim, Ja Seong Bae, Jeong Soo Kim
Scientific Reports.2021;[Epub] CrossRef - A Newly Developed Pancreatic Adenocarcinoma in a Patient with Advanced Thyroid Cancer under Long-Term Sorafenib Use
Min Ji Kim, Han-Sang Baek, Sung Hak Lee, Dong-Jun Lim
International Journal of Thyroidology.2021; 14(2): 175. CrossRef - Modified risk stratification based on cervical lymph node metastases following lobectomy for papillary thyroid carcinoma
Eyun Song, Jonghwa Ahn, Dong Eun Song, Won Woong Kim, Min Ji Jeon, Tae‐Yon Sung, Tae Yong Kim, Ki Wook Chung, Won Bae Kim, Young Kee Shong, Suck Joon Hong, Yu‐Mi Lee, Won Gu Kim
Clinical Endocrinology.2020; 92(4): 358. CrossRef - Long-term scintigraphic and clinical follow up in patients with differentiated thyroid cancer and iodine avid bone metastases
Omnia Mohamed Talaat, Ismail Mohamed Ali, Sherif Maher Abolyazid, Bader Abdelmaksoud, Ibrahim Mansour Nasr
Nuclear Medicine Communications.2020; 41(4): 327. CrossRef - Highly prevalent BRAF V600E and low-frequency TERT promoter mutations underlie papillary thyroid carcinoma in Koreans
Sue Youn Kim, Taeeun Kim, Kwangsoon Kim, Ja Seong Bae, Jeong Soo Kim, Chan Kwon Jung
Journal of Pathology and Translational Medicine.2020; 54(4): 310. CrossRef - Clinical Implication of World Health Organization Classification in Patients with Follicular Thyroid Carcinoma in South Korea: A Multicenter Cohort Study
Meihua Jin, Eun Sook Kim, Bo Hyun Kim, Hee Kyung Kim, Hyon-Seung Yi, Min Ji Jeon, Tae Yong Kim, Ho-Cheol Kang, Won Bae Kim, Young Kee Shong, Mijin Kim, Won Gu Kim
Endocrinology and Metabolism.2020; 35(3): 618. CrossRef - The age threshold of the 8th edition AJCC classification is useful for indicating patients with aggressive papillary thyroid cancer in clinical practice
Krzysztof Kaliszewski, Dorota Diakowska, Łukasz Nowak, Beata Wojtczak, Jerzy Rudnicki
BMC Cancer.2020;[Epub] CrossRef - Lobectomy Is Feasible for 1–4 cm Papillary Thyroid Carcinomas: A 10-Year Propensity Score Matched-Pair Analysis on Recurrence
Eyun Song, Minkyu Han, Hye-Seon Oh, Won Woong Kim, Min Ji Jeon, Yu-Mi Lee, Tae Yong Kim, Ki Wook Chung, Won Bae Kim, Young Kee Shong, Suck Joon Hong, Tae-Yon Sung, Won Gu Kim
Thyroid.2019; 29(1): 64. CrossRef - The binary presence or absence of lymph node metastasis or extrathyroidal extension is not associated with survival in papillary thyroid cancers: Implications for staging systems
Hyun-Soo Zhang, Eun-Kyung Lee, Yuh-Seog Jung, Byung-Ho Nam, Boyoung Park
Cancer Epidemiology.2019; 63: 101589. CrossRef - Risk of Adverse Obstetric Outcomes and the Abnormal Growth of Offspring in Women with a History of Thyroid Cancer
Geum Joon Cho, So-youn Kim, Hoi Chang Lee, Kyu-Min Lee, Sung Won Han, Min-Jeong Oh, Teresa K. Woodruff
Thyroid.2019; 29(6): 879. CrossRef - Changes in Serum Thyroglobulin Levels After Lobectomy in Patients with Low-Risk Papillary Thyroid Cancer
Suyeon Park, Min Ji Jeon, Hye-Seon Oh, Yu-Mi Lee, Tae-Yon Sung, Minkyu Han, Ji Min Han, Tae Yong Kim, Ki-Wook Chung, Won Bae Kim, Young Kee Shong, Won Gu Kim
Thyroid.2018; 28(8): 997. CrossRef - Clinical Outcomes of Differentiated Thyroid Cancer Patients with Local Recurrence or Distant Metastasis Detected in Old Age
Ji Min Han, Ji Cheol Bae, Hye In Kim, Sam Kwon, Min Ji Jeon, Won Gu Kim, Tae Yong Kim, Young Kee Shong, Won Bae Kim
Endocrinology and Metabolism.2018; 33(4): 459. CrossRef - Prognosis of Differentiated Thyroid Carcinoma with Initial Distant Metastasis: A Multicenter Study in Korea
Hosu Kim, Hye In Kim, Sun Wook Kim, Jaehoon Jung, Min Ji Jeon, Won Gu Kim, Tae Yong Kim, Hee Kyung Kim, Ho-Cheol Kang, Ji Min Han, Yoon Young Cho, Tae Hyuk Kim, Jae Hoon Chung
Endocrinology and Metabolism.2018; 33(2): 287. CrossRef - Decreasing Disease-Specific Mortality of Differentiated Thyroid Cancer in Korea: A Multicenter Cohort Study
Min Ji Jeon, Hee Kyung Kim, Eun Heui Kim, Eun Sook Kim, Hyon-Seung Yi, Tae Yong Kim, Ho-Cheol Kang, Young Kee Shong, Won Bae Kim, Bo Hyun Kim, Won Gu Kim
Thyroid.2018; 28(9): 1121. CrossRef - Active Surveillance of Low-Risk Papillary Thyroid Microcarcinoma: A Multi-Center Cohort Study in Korea
Hye-Seon Oh, Jeonghoon Ha, Hye In Kim, Tae Hyuk Kim, Won Gu Kim, Dong-Jun Lim, Tae Yong Kim, Sun Wook Kim, Won Bae Kim, Young Kee Shong, Jae Hoon Chung, Jung Hwan Baek
Thyroid.2018; 28(12): 1587. CrossRef
- Log odds of negative lymph nodes/T stage ratio (LONT): A new prognostic tool for differentiated thyroid cancer without metastases in patients aged 55 and older

- Clinical Study
- The Recovery of Hypothalamic-Pituitary-Adrenal Axis Is Rapid in Subclinical Cushing Syndrome
- Hee Kyung Kim, Jee Hee Yoon, Yun Ah Jeong, Ho-Cheol Kang
- Endocrinol Metab. 2016;31(4):592-597. Published online December 20, 2016
- DOI: https://doi.org/10.3803/EnM.2016.31.4.592
- 3,665 View
- 45 Download
- 8 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background In subclinical Cushing syndrome (SC), it is assumed that glucocorticoid production is insufficient to cause a clinically recognizable syndrome. Differences in hormonal levels or recovery time of the hypothalamic-pituitary-adrenocortical (HPA) axis after adrenalectomy between patients with overt Cushing syndrome (OC) and SC remain unknown.
Methods Thirty-six patients (10 with OC and 26 with SC) with adrenal Cushing syndrome who underwent adrenalectomy from 2004 to 2014 were reviewed retrospectively. Patients were treated with glucocorticoid after adrenalectomy and were reevaluated every 1 to 6 months using a rapid adrenocorticotropic hormone (ACTH) stimulation test.
Results Levels of basal 24-hour urine free cortisol (UFC), serum cortisol after an overnight dexamethasone suppression test (DST), and serum cortisol and 24-hour UFC after low-dose DST and high-dose DST were all significantly lower in patients with SC compared with OC. Basal ACTH levels showed significantly higher in patients with SC compared with OC. The probability of recovering adrenal function during follow-up differed significantly between patients with OC and SC (
P =0.001), with significant correlations with the degree of preoperative cortisol excess. Patients with OC required a longer duration of glucocorticoid replacement to recover a normal ACTH stimulation test compared with patients with SC (median 17.0 months vs. 4.0 months,P <0.001).Conclusion The HPA axis recovery time after adrenalectomy in patients with SC is rapid and is dependent on the degree of cortisol excess. More precise definition of SC is necessary to achieve a better management of patients and to avoid the risk of under- or over-treatment of SC patients.
-
Citations
Citations to this article as recorded by- Hypothalamic–pituitary–adrenal axis recovery after treatment of Cushing's syndrome
Annemarie Balasko, Karin Zibar Tomsic, Darko Kastelan, Tina Dusek
Journal of Neuroendocrinology.2022;[Epub] CrossRef - Early assessment of postoperative adrenal function is necessary after adrenalectomy for mild autonomous cortisol secretion
Trenton Foster, Irina Bancos, Travis McKenzie, Benzon Dy, Geoffrey Thompson, Melanie Lyden
Surgery.2021; 169(1): 150. CrossRef - Is Prophylactic Steroid Treatment Mandatory for Subclinical Cushing Syndrome After Unilateral Laparoscopic Adrenalectomy?
Dong Wang, Han-zhong Li, Yu-shi Zhang, Liang Wang, Zhi-gang Ji
Surgical Laparoscopy, Endoscopy & Percutaneous Techniques.2019; 29(1): 31. CrossRef - When to Intervene for Subclinical Cushing's Syndrome
Lily B. Hsieh, Erin Mackinney, Tracy S. Wang
Surgical Clinics of North America.2019; 99(4): 747. CrossRef - Serum Cortisol Levels via Radioimmunoassay vs Liquid Chromatography Mass Spectrophotometry in Healthy Control Subjects and Patients With Adrenal Incidentalomas
Martha K P Huayllas, Brian C Netzel, Ravinder J Singh, Claudio E Kater
Laboratory Medicine.2018;[Epub] CrossRef - Contralateral adrenal width predicts the duration of prolonged post‐surgical steroid replacement for subclinical Cushing syndrome
Masahiro Sugiura, Yusuke Imamura, Koji Kawamura, Satoshi Yamamoto, Tomokazu Sazuka, Kazuyoshi Nakamura, Shinichi Sakamoto, Hidekazu Nagano, Hisashi Koide, Tomoaki Tanaka, Takashi Imamoto, Akira Komiya, Tomohiko Ichikawa
International Journal of Urology.2018; 25(6): 583. CrossRef - Predictability of hypoadrenalism occurrence and duration after adrenalectomy for ACTH-independent hypercortisolism
V. Morelli, L. Minelli, C. Eller-Vainicher, S. Palmieri, E. Cairoli, A. Spada, M. Arosio, I. Chiodini
Journal of Endocrinological Investigation.2018; 41(4): 485. CrossRef - Articles inEndocrinology and Metabolismin 2016
Won-Young Lee
Endocrinology and Metabolism.2017; 32(1): 62. CrossRef
- Hypothalamic–pituitary–adrenal axis recovery after treatment of Cushing's syndrome


 KES
KES

 First
First Prev
Prev



